Women are nearly four times more likely to develop an Autoimmune Disease than men. That is significant yet rarely discussed as seriously as it should be. Very interestingly it is the inherent strength of woman’s stronger immune system that is often the culprit.
As we research further at Auragens, whatever the cause of the symptom, the results are a diminished quality of life for the women afflicted. But many of these issues may be successfully treated with hu-MSC stem cell treatments. Yet, the female demographic is rarely spoken to or educated on this fact.
In an effort to educate and open up the conversation we are going to address the reasons why women are more likely to deal with an autoimmune disease as well as the reason behind the success of stem cell treatments in dealing with the issue.
Why Are Women More Susceptible to Autoimmune Disease?
Women are more susceptible to autoimmune diseases due to a combination of genetic, hormonal, and environmental factors. The key points are:
1️⃣ Genetic Factors:
-
X Chromosome: Women have two X chromosomes, while men have one X and one Y chromosome. The X chromosome contains many genes related to the immune system. This can lead to a more robust immune response, which, while beneficial in fighting infections, can also increase the risk of the immune system attacking the body’s own tissues.
-
Gene Variants: Certain gene variants associated with autoimmune diseases are more prevalent or expressed differently in women, contributing to a higher risk.
2️⃣ Hormonal Influences:
-
Estrogen: The female hormone estrogen has a complex influence on the immune system. It can enhance immune responses, which might lead to a higher incidence of autoimmune diseases. For instance, fluctuations in estrogen levels during menstrual cycles, pregnancy, and menopause can affect disease activity.
-
Prolactin: This hormone, which is higher in women, especially during pregnancy and breastfeeding, also stimulates the immune system and may contribute to the development of autoimmune diseases.
3️⃣ Immune System Differences:
-
Innate and Adaptive Immunity: Women generally have a stronger innate and adaptive immune response compared to men. While this makes women better at combating infections, it also means their immune systems are more likely to become overactive and attack their own tissues.
-
Cytokine Production: Women tend to produce higher levels of certain cytokines (signaling proteins in the immune system) that can promote inflammation, a key feature in many autoimmune diseases.
4️⃣ Environmental and Lifestyle Factors:
-
Infections: Certain infections can trigger autoimmune responses. The way women respond to these infections, influenced by their hormonal and genetic makeup, might increase the likelihood of developing an autoimmune disease.
-
Stress: Chronic stress can affect the immune system, and women may experience and process stress differently than men, potentially influencing autoimmune disease development.
5️⃣ Epigenetic Factors:
-
Gene Expression Regulation: Epigenetic changes, which affect how genes are turned on or off without altering the DNA sequence, can be influenced by hormonal and environmental factors. These changes can play a significant role in the susceptibility to autoimmune diseases and might differ between men and women.
Examples of Autoimmune Diseases More Common in Women:
-
Systemic Lupus Erythematosus (SLE): Women are affected about nine times more often than men.
-
Rheumatoid Arthritis (RA): Women are affected about two to three times more often than men.
-
Multiple Sclerosis (MS): Women are affected about two to three times more often than men.
Overall, the interplay between genetic predisposition, hormonal influences, and immune system differences underlies the higher prevalence of autoimmune diseases in women.

Stem Cell Treatments for Autoimmune Diseases Human mesenchymal stem cells (hu-MSCs) have shown effectiveness in treating autoimmune diseases due to their unique properties and mechanisms of action. Here are some key reasons why hu-MSC treatments are effective in addressing autoimmune diseases:
1️⃣ Immunomodulation:
-
Immune System Regulation: hu-MSCs have the ability to modulate the immune system. They can reduce the activity of overactive immune cells and promote the generation of regulatory T cells (Tregs), which help maintain immune tolerance and prevent autoimmune reactions.
-
Cytokine Secretion: hu-MSCs secrete anti-inflammatory cytokines such as IL-10, TGF-β, and prostaglandin E2. These cytokines help reduce inflammation and suppress the immune response that contributes to autoimmune diseases.
2️⃣ Anti-inflammatory Effects:
-
Reduction of Inflammation: hu-MSCs can migrate to sites of inflammation and release factors that inhibit inflammatory processes. This can help reduce the chronic inflammation associated with autoimmune diseases, leading to symptom relief and tissue repair.
-
Inhibition of Pro-inflammatory Cells: hu-MSCs can inhibit the proliferation and activity of pro-inflammatory immune cells like Th17 cells and macrophages, which play a significant role in autoimmune pathology.
3️⃣ Tissue Repair and Regeneration:
-
Promotion of Healing: hu-MSCs have the ability to promote tissue repair and regeneration. They can differentiate into various cell types, such as bone, cartilage, and muscle cells, aiding in the repair of damaged tissues caused by autoimmune attacks.
-
Paracrine Effects: hu-MSCs release a variety of growth factors and bioactive molecules that support tissue healing and regeneration, improving the function of affected organs and tissues
4️⃣ Homing and Engraftment:
-
Targeted Migration: hu-MSCs have the capacity to home to sites of tissue damage and inflammation. This targeted migration allows them to exert their therapeutic effects directly at the sites of autoimmune activity.
-
Temporary Engraftment: While hu-MSCs may not permanently engraft in the tissues, their temporary presence is sufficient to modulate the immune response and initiate repair processes.
5️⃣ Low Immunogenicity:
-
Minimal Immune Rejection: hu-MSCs have low immunogenicity, meaning they are less likely to be recognized and attacked by the host’s immune system. This makes them suitable for allogeneic (donor-derived) transplantation, expanding their therapeutic potential.
6️⃣ Safety Profile:
-
Favorable Safety: hu-MSCs have a favorable safety profile in clinical applications. They are generally well-tolerated and have a low risk of adverse effects, making them a promising option for long-term treatment of autoimmune diseases.

Clinical Applications:
-
Rheumatoid Arthritis (RA): hu-MSCs have been shown to reduce inflammation and improve joint function in RA patients.
-
Systemic Lupus Erythematosus (SLE): hu-MSCs can help modulate the immune system and reduce lupus-related tissue damage.
-
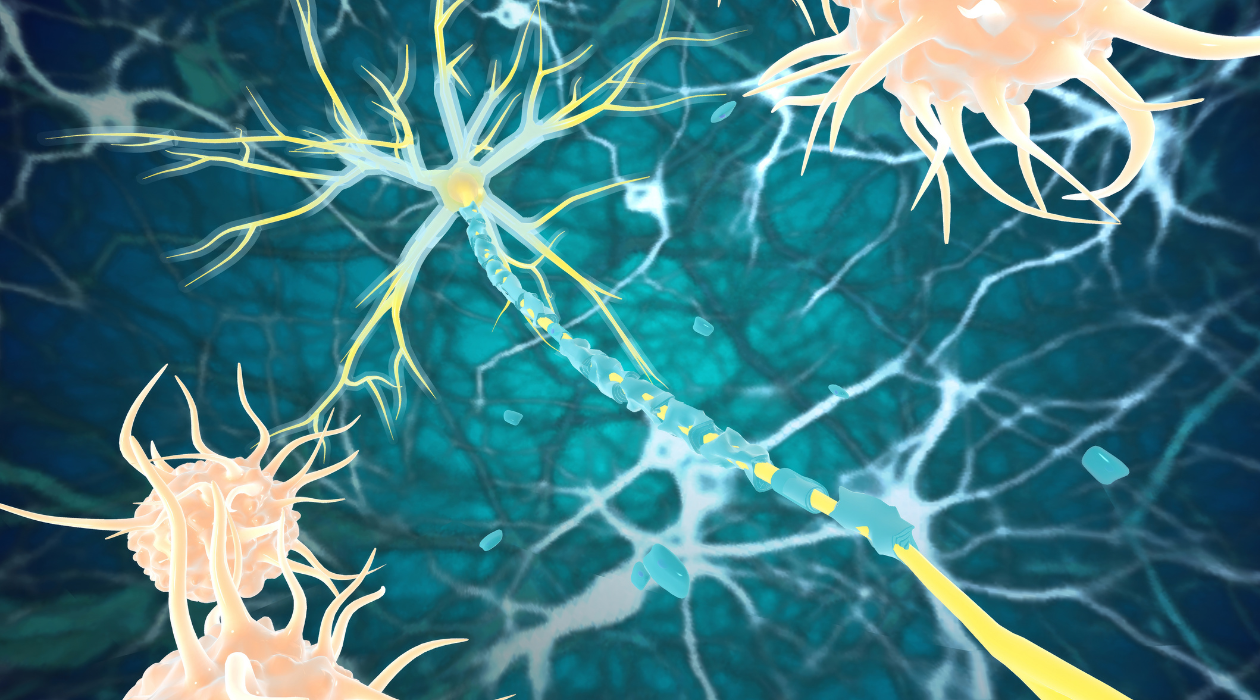
Multiple Sclerosis (MS): hu-MSCs may promote neural repair and reduce neuroinflammation in MS patients.