Posted July 10, 2024
Abstract
Chronic lumbar pain associated to multiple conditions including discopathy and facet arthropathy can significantly impact a patient’s quality of life requiring innovative treatment approaches that are safe, effective, and sustainable. This case study evaluates the safety and efficacy of regenerative medicine biologic products in the form of human umbilical cord Wharton’s Jelly derived mesenchymal stromal cells (hUC-MSC) and exosomes delivered intravenously and locally via erector spinae plane (ESP) block, for the relief of chronic lumbar pain.
Patients in this case review were treated via intravenous (IV) and local injections as protocolized by Auragens Clinic and were assessed prior to treatment and post treatment using the Visual Analogue Scale (VAS) to assess safety and efficacy of the intervention.
Our findings suggest that hUC-MSC cell therapies and exosome-based therapies are safe and significantly reduce pain, supporting their use as promising modalities for chronic pain management, opening opportunities for further investigation to elucidate clinical efficacy and specify indications for use.
Keywords
Mesenchymal Stromal Cells (MSC); Regenerative Medicine; Discopathies; Chronic Lumbar Pain; Visual Analogue Scale (VAS); Flow Cytometry; Electron Microscopy; Extracellular Vesicles (EVs); Erector Spinae Plane (ESP) Block; MSC-Derived Exosomes; Analgesia; Pain Management; Paravertebral Space; Epidural Space; Biologic Therapies; Case Report Series.
Copyright 2024
Genesis pub by Diaz C, et al. CC BY-NC-ND 4.0 DEED. This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-No Derivatives 4.0 International License.,This allows others distribute, remix, tweak, and build upon the work, even commercially, as long as they credit the authors for the original creation.
Abstract
Chronic lumbar pain associated to multiple conditions including discopathy and facet arthropathy can significantly impact a patient’s quality of life requiring innovative treatment approaches that are safe, effective, and sustainable. This case study evaluates the safety and efficacy of regenerative medicine biologic products in the form of human umbilical cord Wharton’s Jelly derived mesenchymal stromal cells (hUC-MSC) and exosomes delivered intravenously and locally via erector spinae plane (ESP) block, for the relief of chronic lumbar pain.
Patients in this case review were treated via intravenous (IV) and local injections as protocolized by Auragens Clinic and were assessed prior to treatment and post treatment using the Visual Analogue Scale (VAS) to assess safety and efficacy of the intervention.
Our findings suggest that hUC-MSC cell therapies and exosome-based therapies are safe and significantly reduce pain, supporting their use as promising modalities for chronic pain management, opening opportunities for further investigation to elucidate clinical efficacy and specify indications for use.
Keywords
Mesenchymal Stromal Cells (MSC); Regenerative Medicine; Discopathies; Chronic Lumbar Pain; Visual Analogue Scale (VAS); Flow Cytometry; Electron Microscopy; Extracellular Vesicles (EVs); Erector Spinae Plane (ESP) Block; MSC-Derived Exosomes; Analgesia; Pain Management; Paravertebral Space; Epidural Space; Biologic Therapies; Case Report Series.
Introduction
Chronic lumbar pain is a prevalent and debilitating progressive condition often resulting from discopathies, facet joint arthropathies, or other underlying spinal disorders. Conventional treatments for pain management are mainly limited to pharmaceutical analgesics, physical therapy and in some cases surgical intervention, often these modalities fail or do not provide long-term relief. Many times, these options are unsustainable for patients that may experience adverse effects associated to medication or who may not be candidate for corrective surgeries, this underscores the need for novel approaches.
Regenerative medicine is a growing field in biomedical and clinical practices which seeks to harness the biologic output of living cells and extracellular vesicles to replace or improve the function of damaged tissues.
Mesenchymal stromal cells from varying sources have recently gained much attention in the field given the noteworthy anti-inflammatory, immune-modulatory and regenerative characteristics of their extracellular vesicles (EVs) also know as exosomes. Wharton’s Jelly derived MSC have championed therapeutic strategies for chronic pain and inflammatory pathologies as they are easily isolated and ethically harvested from perinatal tissues which are otherwise considered medical or biologic “waste”. Also of importance, exosomes play a crucial role in cell-cell communication and could be key in mediating the regenerative processes necessary for pain relief.
The erector spinae plane block (ESP) is a relatively new technique in regional anesthesia and pain management that has proven of great benefit for short term pain relief and post-operatory pain management. This procedure targets the fascial plane between the erector spinae muscle and transverse processes of the vertebrae. While the exact mechanism of action is not fully understood, evidence indicates a diffusion of local anesthetic into adjacent paravertebral and epidural spaces. This diffusion likely influences both somatic and sympathetic pain pathways, effectively impeding the transmission of pain signals from the dorsal and ventral rami of spinal nerves to the central nervous system [1]. This procedure has been effectively used in various surgical contexts, such as thoracic, breast and orthopedic surgery, highlighting its versatility and efficacy in pain management including post operative pain control after spine surgery [2-4].
Our treatment protocol integrates the ESP block technique replacing local anesthetics with mesenchymal stromal cell products leveraging the targeted delivery and therapeutic effects respectively to treat patients with chronic lumbar pain aiming to achieve a more sustainable pain relief through regenerative medicine.
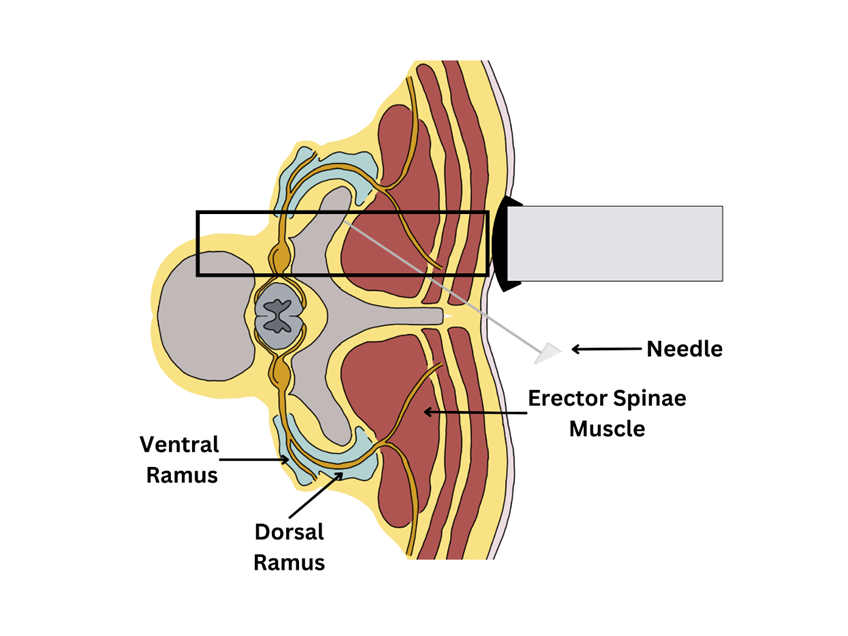
Figure 1.
A visual depiction of the ESP block technique: the needle is being guided by ultrasound between the erector spinae muscle group and the transverse process. Once it reaches the transverse process, local anesthetic solution is administered.
Methods & Protocol Design
This case report series was conducted to describe the safety and efficacy of MSC administered intravenously along with exosomes delivered via ESP infiltration for the management of chronic lumbar spinal pain. The case report series details the medical histories, treatment protocols and post-treatment follow-up evaluations using the VAS to assess pain levels and functional outcomes of four patients labeled Patients A, B, C, and D in this study.
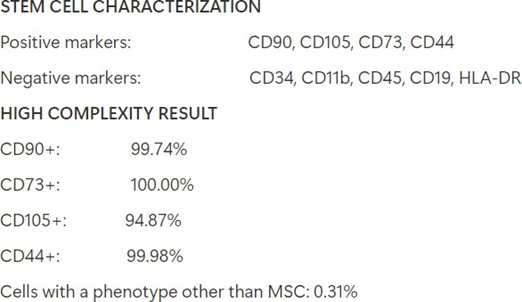
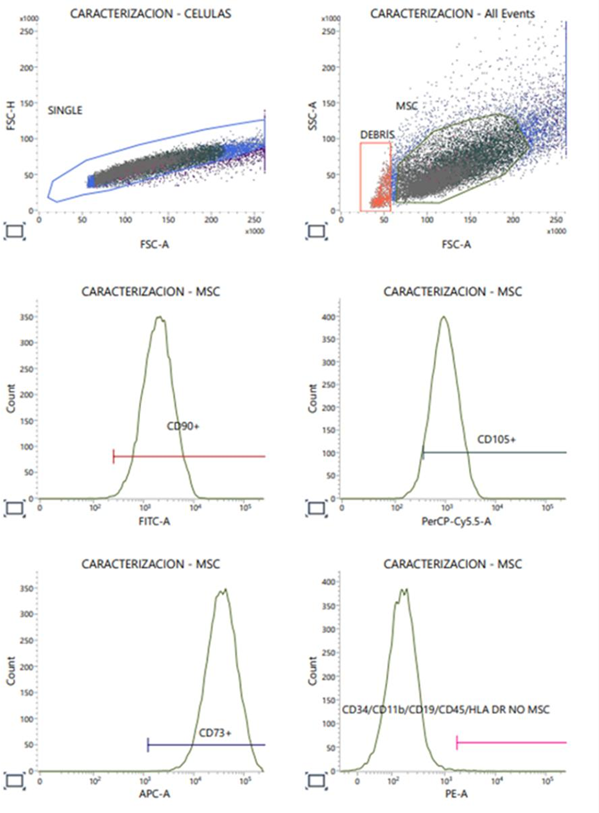
The isolation of MSC from human umbilical cord involved a series of steps with stringent quality control measures to ensure the safety and efficacy of the cells for clinical application. These steps were conducted in a GMP-grade ISO7 cleanroom in accordance with the International Cellular Therapy (ISCT) guidelines. Collection, dissection, enzymatic digestion, filtration and centrifugation as well as culture expansion and harvesting were all performed at Auragens Laboratory facility. MSC were characterized using flowcytometry to confirm surface expression markers (CD90, CD105, CD73, and CD44) and the absence of hematopoietic markers (CD34, CD11b, CD45, CD19) and HLA-DR. Quality control criteria were measured via viability quantification, sterility and endotoxin testing, cryopreservation, thawing and syringe preparation. MSC-derived exosomes were isolated and purified from the culture media of these cells using ultracentrifugation techniques and quantified using electron microscopy and size exclusion criteria of 80 to 130nm in size.
This methodology provides a detailed blueprint for investigating the efficacy of MSC and MSC- derived exosomes in treating chronic spinal pain through ESP blocks. This descriptive analysis aims to contribute valuable data to the field of regenerative medicine, offering insights into new pain management strategies for patients with discopathies.
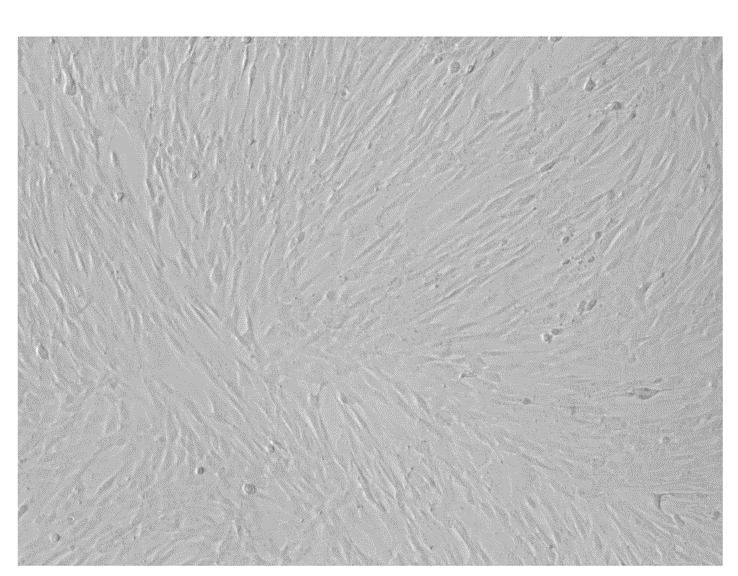
Image 1.
Human umbilical cord mesenchymal stem cells (hUC-MSC) observed under optical microscopy day 36 of culture expansion.
Treatment Protocol
The intervention involved the delivery of MSC via intravenous (IV) infusion at a dose of 1-2 million hUC-MSC per kilogram of patients’ total bodyweight. This dose was administered as 50 x 10^6 hUC-MSC IV per day for a total of 3 days (except for two patients who received treatment for 4 days due to total IV dose of 200 x 10^6 hUC-MSC). The ESP infiltration was performed within a sterile environment, with patients positioned prone for enhanced access. Utilizing an ultrasound curved array probe, the lumbar transverse processes were accurately identified bilaterally. The ESP infiltrations were performed under real-time ultrasound guidance, ensuring precise echogenic needle placement and direct-site location of the biologic agents. Subsequently, 5 ml of 1% lidocaine solution was administered to provide superficial anesthesia to the subcutaneous tissues. Following this, a combination of 1 exosome cryovial containing 10×10^9 micro-vesicles in 1mL and 20 ml of normal saline solution (NSS), was carefully injected into the fascial plane above the tip of the transverse process of the vertebrae of each side. The diffusion along the erector spinae fascia was evidenced by the ultrasound image, also allowing for diligent monitoring ensured continuous visualization of the needle tip, ensuring utmost safety and precision.
Outcome Measures
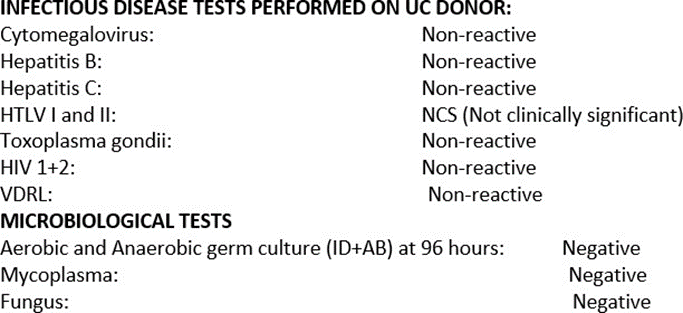
The primary outcome measures were pain relief or change, assessed using the Visual Analogue Scale (VAS). The VAS is a unidimensional measure of pain intensity, which has been widely used in diverse adult populations, including those with chronic pain.
Visual Analogue Scale (VAS): Patients were asked to mark their pain level on 0 to 10 scale representing a continuum from “no pain” to “worst pain imaginable.”
Image 2.
Visual Analogue Scale (VAS) Brookbush Institute.
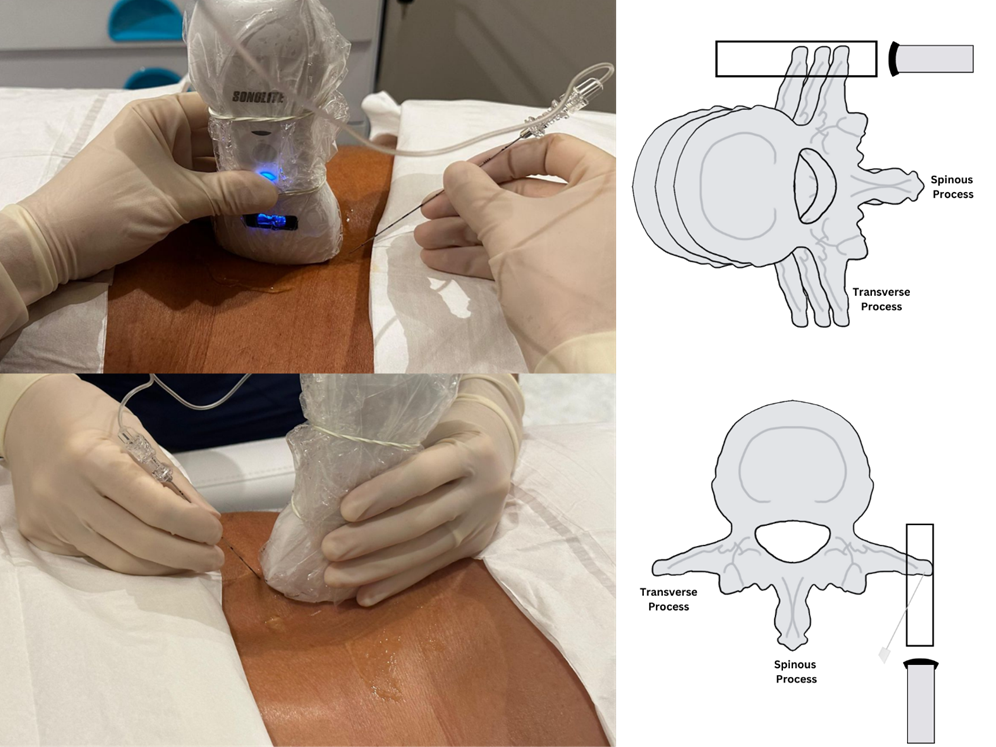
Image 3.
The procedure was executed within a sterile environment, with patients positioned prone for enhanced access. Utilizing an ultrasound curved array probe, the lumbar transverse processes were accurately identified bilaterally.
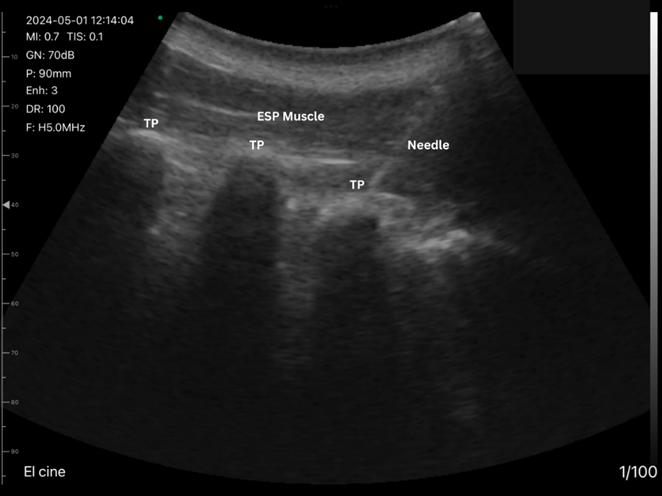
Image 4.
The ESP infiltrations were performed under real-time ultrasound guidance, ensuring precise echogenic needle placement and direct-site location of the biologic agents. TP (Transverse Process) ESP (Erector Spinae Plane Muscle).
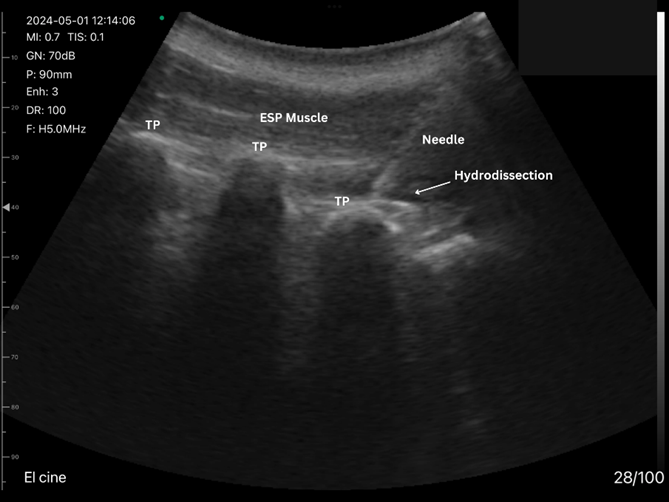
Image 5.
The diffusion along the erector spinae fascia was evidenced by the ultrasound image also allowing for diligent monitoring ensured continuous visualization of the needle tip, ensuring utmost safety and precision. TP (Transverse Process) ESP (Erector Spinae Plane Muscle).
Follow-Up And Data Collection
Patients were followed-up at different time points post-procedure to assess the long-term effects of the treatment. Each follow-up involved clinical evaluations, and completion of the VAS Score. Adverse events related to the procedure or the MSC and exosome therapy were also recorded and analyzed.
Statistical Analysis
Descriptive analysis was used to summarize patient demographics and baseline characteristics. Changes in VAS scores over time were analyzed and compared and charted in their Electronic History Record (EHR).
Ethical Considerations
The umbilical cords were donated by pregnant patients under informed consent, rigorously evaluated and tested for metabolic, genetic and infectious diseases during the 2nd and 3rd trimester of gestation.
Patients consented to treatment protocol after evaluation and explanation and were made aware of the investigational nature of the procedures whilst managing expectations for improvement.
Results
Patient A
A 51-year-old male with a history of chronic lumbar pain associated with L3-L4 Degenerative Disc Disease. The patient reported a pre-treatment VAS score of 8/10, with unbearable pain while walking short distances and radiculopathy radiating to both lower limbs when standing up from a chair. He was taking oral analgesics including gabapentin 600mg per day and meloxicam as needed.
-
Treatment Protocol
Patient A received 200 million human umbilical cord-derived mesenchymal stromal cells (hUC- MSC) intravenously, fractioned into 50 million cells daily over a four-day period. Additionally, he underwent treatment with 10 x 10^9 exosomes suspended in 20 mL of normal saline solution (NSS), administered via lumbar erector spinae plane (ESP) infiltration.
-
Response to Treatment
Following the treatment regimen, Patient A reported a significant decrease in pain levels. Pain scores, initially severe, decreased to a 0/10 VAS at several follow-up intervals 1-6-9months post-treatment. The patient experienced improved mobility and no longer required gabapentin or meloxicam for pain management. He resumed routine daily activities three days post-procedure, with no short or long-term complications reported. The patient continues to benefit from the procedure with no reported reversal or change in symptoms.
Patient B
A 56-year-old male with a history of chronic lumbar pain. The patient reported a pre-treatment VAS score of 7/10, with pain occurring after exertion or when laying on his back. He did not report taking any medications for pain management.
-
Treatment Protocol
Patient B received 150 million human umbilical cord-derived mesenchymal stromal cells (hUC- MSC) intravenously, fractioned into 50 million cells daily over a three-day period. Additionally, he underwent treatment with 10 x 10^9 exosomes suspended in 20 mL of normal saline solution (NSS), administered via lumbar erector spinae plane (ESP) infiltration.
-
Response to Treatment
Following the treatment regimen, Patient B reported a significant improvement in pain levels. Pain scores, initially severe, decreased to a 2/10 VAS post-treatment. The patient experienced improved mobility and did not require any additional or new medications for pain management. He resumed routine daily activities one day post-procedure, with no short or long-term complications reported. The patient continues to benefit from the procedure, reporting being pain-free 10 months post-treatment.
The outcomes observed in Patient B suggest that hUC-MSC and exosomes may offer promising benefits in managing chronic lumbar pain. The targeted delivery of exosomes via lumbar ESP infiltration, in addition to systemic administration of hUC-MSC, may have contributed to the observed clinical improvements. This dual approach potentially addresses both systemic and localized sources of pain and pathology. These therapies are hypothesized to exert anti- inflammatory and regenerative effects, potentially addressing the underlying pathologies associated with chronic lumbar pain.
Patient C
A 53-year-old male with a history of chronic lumbar pain associated with a T12/L1 lateral protrusion with annular fissuring of the intervertebral disc, moderate canal stenosis, L2 stable hemangioma, and L4/L5 retrolisthesis. The patient reported a pre-treatment VAS score of 10/10, with pain radiating along the right lower limb and paresthesia along the lateral aspect of the left thigh, taking hydrocodone/acetaminophen compound, and oral ketorolac daily pain management.
-
Treatment Protocol
Patient C received 150 million human umbilical cord-derived mesenchymal stromal cells (hUC- MSC) intravenously, fractioned into 50 million cells daily over a three-day period. Additionally, he underwent treatment with 10 x 10^9 exosomes suspended in 20 mL of normal saline solution (NSS), administered via lumbar erector spinae plane (ESP) infiltration.
-
Response to Treatment
Following the treatment regimen, Patient C reported a significant improvement in pain levels. Pain scores, initially severe, decreased to a 1/10 VAS at follow-up evaluation 12 months post-treatment. The patient experienced improved mobility and discontinued the use of hydrocodone and ketorolac, occasionally using over-the-counter NSAIDs for mild pain. He resumed routine daily activities one-week post-procedure, with no short or long-term complications reported. The patient continues with tolerable symptoms 12 months post-treatment and has resumed daily activities, including MMA sparring and weightlifting.
Patient D
A 52-year-old male with chronic lumbar pain attributed to degenerative disc disease at L2-L3 and a right disc protrusion at L5/S1. His pre-treatment VAS pain score was 7/10, with pain localized to the lumbar spine during exertion and without radiculopathy managing his symptoms with celecoxib daily oral use.
-
Treatment Protocol
Patient D underwent the following treatment regimen: He received 200 million human umbilical cord-derived mesenchymal stromal cells (hUC-MSC) intravenously, fractioned into 50 million cells per day over four days. Additionally, he received 5 million hUC-MSC infiltrated into the L4- L5-S1 facet joints and 20 x 10^9 exosomes in 30 mL of normal saline solution (NSS) via lumbar Erector Spinae Plane (ESP) infiltration.
-
Response to Treatment
Following the procedures, Patient D reported no short or long-term complications. He resumed routine daily activities two days post-procedure. Follow-up evaluations conducted post-treatment consistently showed a VAS pain score of 3/10. Patient D discontinued the use of pain medications, and he reported improvement in mobility and flexibility at six months post-treatment, with no reversal of symptoms (Table 1).
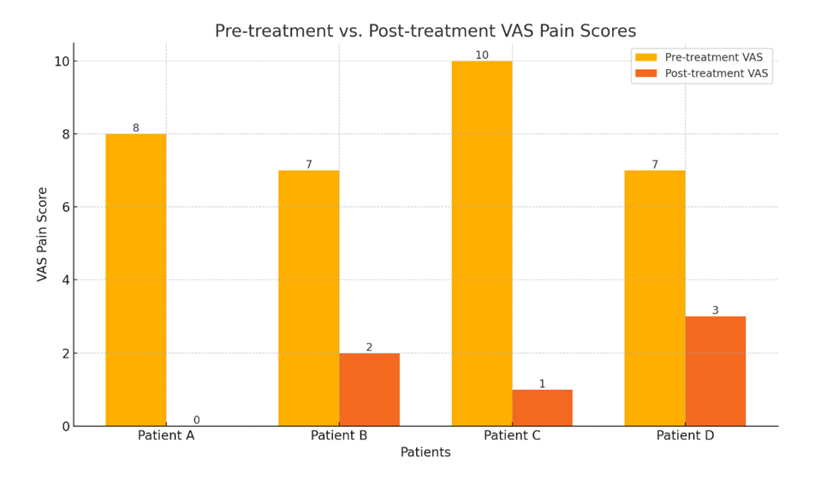
Table 1.
The percentage of recovery for each patient, based on the reduction in VAS pain scores, is as follows:
-
Patient A: 100%
-
Patient B: 71.43%
-
Patient C: 90%
-
Patient D: 57.14%
The median percentage of recovery across all patients was 80.71%.
This indicates that the median patient experienced an approximate 80.71% reduction in their VAS pain score following treatment.
Discussion
Chronic lumbar pain remains a prevalent and debilitating condition, affecting millions worldwide. Traditional treatment modalities often fall short in providing sustained relief and are frequently accompanied by undesirable side effects. The search for more effective and less invasive treatments has led to the exploration of novel therapies, such as mesenchymal stromal cells (MSC), known for their regenerative and anti-inflammatory properties. This discussion examines the potential of combining Erector Spinae Plane (ESP) infiltration with MSC to manage chronic lumbar pain.
The outcomes observed in all four patients suggest that combined hUC-MSC and exosome therapy may offer significant benefits in managing complex lumbar pain associated with multiple spinal pathologies. This treatment approach resulted in effective pain relief and functional improvement, allowing for the discontinuation of routine analgesic medications. Further research with larger patient populations and longer-term follow-up is necessary to confirm these findings and optimize treatment protocols. Safety outcomes were also evaluated, none of the patients experienced short or long-term adverse reactions to systemic or localized treatments with MSC and MSC-derived exosomes.
The Erector Spinae Plane (ESP) Block
The ESP block, introduced as a regional anesthesia technique, has gained popularity due to its versatility, safety, and efficacy in pain management. By injecting local anesthetics into the fascial plane between the erector spinae muscle and the transverse processes of the vertebrae, the ESP block effectively provides analgesia. This technique has been shown to be beneficial in various surgical and chronic pain scenarios, such as thoracic, breast and orthopedic surgery, highlighting its versatility and efficacy in pain management including post operative pain control after spine surgery offering substantial pain relief while minimizing opioid consumption (4). Given the evidence of the erector spinae plane block, we employed targeted delivery of mesenchymal stem cells to harness its mechanism of action replacing local anesthetic for MSC exosomes.
Mesenchymal Stromal Cells (MSC) In Pain Management
MSC are multipotent cells with the capability to differentiate into various cell types and exert immunomodulatory effects. Their therapeutic potential in pain management is largely attributed to their ability to secrete bioactive molecules, including cytokines and growth factors, which promote tissue regeneration and modulate the immune response. These properties make MSC a promising candidate for treating chronic inflammatory conditions and neuropathic pain.
Research has indicated that MSC and their exosomes, can effectively reduce pain by downregulating pro-inflammatory cytokines and upregulating anti-inflammatory cytokines. Animal models of neuropathic pain have shown significant reductions in pain behaviors following exosome administration, highlighting its potential for long-term pain relief and tissue repair [5].
Mesenchymal Stromal Cells (MSC) In Pain Management
MSC are multipotent cells with the capability to differentiate into various cell types and exert immunomodulatory effects. Their therapeutic potential in pain management is largely attributed to their ability to secrete bioactive molecules, including cytokines and growth factors, which promote tissue regeneration and modulate the immune response. These properties make MSC a promising candidate for treating chronic inflammatory conditions and neuropathic pain.
Research has indicated that MSC and their exosomes, can effectively reduce pain by downregulating pro-inflammatory cytokines and upregulating anti-inflammatory cytokines. Animal models of neuropathic pain have shown significant reductions in pain behaviors following exosome administration, highlighting its potential for long-term pain relief and tissue repair [5].
Synergistic Potential Of ESP Infiltration And MSC Therapy
Combining ESP block technique with MSC therapy offers a novel approach to managing chronic lumbar pain. MSC contribute to long-term pain management with potential reparative effect through their regenerative and anti-inflammatory secretions. This targeted fascial plane infiltration with MSC exosomes could potentially enhance the overall efficacy of pain management strategies by addressing both immediate and underlying pathological processes. Preclinical studies suggest that MSC can potentiate the analgesic effects of nerve blocks by promoting nerve regeneration and reducing local inflammation. The use of exosomes in conjunction with ESP infiltration could extend the duration of analgesia and improve functional outcomes in patients with chronic lumbar pain.
Challenges And Future Directions
Despite the promising potential of ESP infiltration combined with MSC therapy, several challenges must be addressed. These include optimizing the dosage and delivery methods for MSC, understanding the long-term safety of repeated MSC administrations, and conducting comprehensive clinical trials in a more heterogenous population to validate the efficacy of this combined approach and detail diagnostic indications for its use. Our understanding of systemic MSC therapy relies on their capacity to provide immunomodulation, modify macrophage phenotypes and produce stimulatory factors via the paracrine effect, that said more understanding regarding the mechanisms, biodistribution and duration of the effects are needed to better support its complementary use.
Future research should focus on elucidating the mechanisms underlying MSC fascial plane infiltration therapy, developing standardized clinical protocols, and exploring MSC derived from various sources, such as bone marrow, adipose tissue, and umbilical cord. Additionally, investigations into the cost-effectiveness and patient accessibility of this combined treatment are essential for its broader adoption in clinical practice.
The integration of ESP infiltration with MSC therapy represents a novel and promising approach to the management of chronic lumbar pain. This combined strategy leverages the long-term regenerative and anti-inflammatory benefits of MSC, offering a comprehensive solution for patients suffering from chronic lower back pain. Ongoing research and clinical trials are crucial to fully understand and harness the potential of this innovative treatment modality, paving the way for improved patient outcomes and quality of life.
CONCLUSION
Our investigation into the use of MSC and derived exosomes for treating chronic lumbar pain through erector spinae infiltrations indicates a significant potential for these therapies in clinical pain management. The results demonstrated notable improvements in pain scores and patient functionality, suggesting an effective strategy for long-term pain control. This study underscores the need for larger, controlled trials to confirm these findings and to further elucidate the mechanisms by which MSC and exosomes exert their analgesic effects. The integration of regenerative medicine into the treatment repertoire for chronic pain could fundamentally alter the therapeutic landscape, offering new hope to patients with chronic discopathies.
References
- Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. (2016) The Erector Spinae Plane Block: A Novel Analgesic Technique in Thoracic Neuropathic Pain. Reg Anesth Pain Med. 41(5):621-27.
- van den Broek RJC, van Meegen VMM, Al Khawaja H, Bouwman AR. (2023) Erector spinae plane block improves postoperative recovery after laminectomy and discectomy surgery: a retrospective cohort study. BMC Anesthesiol 23(1):308.
- Hamilton DL, Manickam B, Perrin D. (2018) A Continuous Erector Spinae Plane Block for Postoperative Pain Management after Minimally Invasive Repair of Pectus Excavatum: A Case Report. A&A Practice. 11(3):67-69.
- Gürkan Y, Aksu C, Kuş A, Yörükoğlu UH. (2020) Erector spinae plane block and thoracic paravertebral block for breast surgery compared to IV-morphine: A randomized controlled trial. J Clin Anesth. 59:84–88.
- Nazemi S, Amini K, Soroush L. (2024) Preemptive administration of mesenchymal stem cells-derived conditioned medium can attenuate the development of neuropathic pain in rats via downregulation of proinflammatory cytokines. Behav Brain Res. 461:114858.
- Drobiova H, Sindhu S, Ahmad R, Haddad D, Al-Mulla F, et al. (2023) Wharton’s jelly mesenchymal stem cells: A concise review of their secretome and prospective clinical applications. Front Cell Dev Biol. 11:1211217.
- Fan C-G, Zhang Ǫ-J, Zhou J-R. (2010) Therapeutic potentials of mesenchymal stem cells derived from human umbilical cord. Stem Cell Rev Rep. 7(1):195-207.
- Zhou Y, Xu H, Xu W. (2020) Effects of Wharton’s jelly-derived mesenchymal stem cell treatment on the pain behavior of a rat model of chronic prostatitis. Pain Physic. 23:E71- E79.
- Chin KJ, El-Boghdadly K. (2021) Mechanisms of action of the erector spinae plane (ESP) block: A narrative review. Can J Anesth. 68(3):387–408.
- Jain K, Jaiswal V, Puri A. (2018) Erector spinae plane block: Relatively new block on horizon with a wide spectrum of application – A case series. Indian J Anaesth. 62(10):809-13.
- Wang L-T, Lee W, Liu K-J, Sytwu H-K, Yen M-L, et al. (2024) Mesenchymal stromal/stem cells (MSC) know best: The remarkable complexities of its interactions with polymorphonuclear neutrophils (PMNs). Stem Cells. 42(5):403-15.
- De Cassai A, Geraldini F, Freo U, Boscolo A, Pettenuzzo T, et al. (2023) Erector Spinae Plane Block and Chronic Pain: An Updated Review and Possible Future Directions. Biology. 12(8):1073.
- Hong JH, Shin SH, Cho EY. (2022) Erector spinae plane block in patients with low back pain. Keimyung Med J. 41(2):103–07.
ARTICLE INFORMATION
DOI
http://https//doi.org/10.52793/JSCR.2024.5(2)-60
Copyright
The copyright holder has placed this preprint in the Public Domain. It is no longer restricted by copyright. Anyone can legally share, reuse, remix, or adapt this material for any purpose without crediting the original authors.
AUTHOR INFORMATION
Christian Díaz1, Manuel Padrón2, Vielka Benedito3, María Regis3, Catalina Gormaz3, Michelle Flores4, Yina Mojica4, Lisbeth Pineda4, Carlos Bracho4, Daniel Briggs5 and Carlos Díaz-Urriola6
1Medical Director, Auragens Clinic Program
2Medical Specialist – Anaesthesiology, Auragens Clinic Program
3Clinic Staff, Auragens Clinic Program
4Biotechnologist/Medical Technologist, Auragens Laboratory Program
5Chief Executive Officer, Auragens Clinic/Laboratory Program
6Chief Medical Officer/Laboratory Directory, Auragens Clinic/Laboratory Program
*Corresponding author: Dr. Christian Diaz, Medical Director, Auragens Clinical Program
Citation: Diaz C, Padron M, Benedito V, Regis M, Gormaz C, et al. (2024) Erector Spinae Infiltration with Mesenchymal Stromal Cells in Chronic Lumbar Pain: A Case Report Series. J Stem Cell Res. 5(2):1-16.
Received: June 10, 2024 | Published: July 10, 2024
Copyright© 2024 genesis pub by Diaz C, et al. CC BY-NC-ND 4.0 DEED. This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-No Derivatives 4.0 International License. This allows others distribute, remix, tweak, and build upon the work, even commercially, as long as they credit the authors for the original creation.