Revolutionizing Autoimmune Treatment with Advanced Stem Cell Therapy at Auragens
CROHN’S | DERMATOMYOSITIS | DEVIC DISEASE | DIABETES (TYPE I) | DIABETES (TYPE II) | HASHIMOTO’S | LYME | MYASTHENIA GRAVIS (MG) | MOTOR NEURON DISEASE (MND) | PEMPHIGUS | POLYMYOSITIS | PSORIASIS | RHEUMATOID ARTHRITIS (RA) | SCLERODERMA
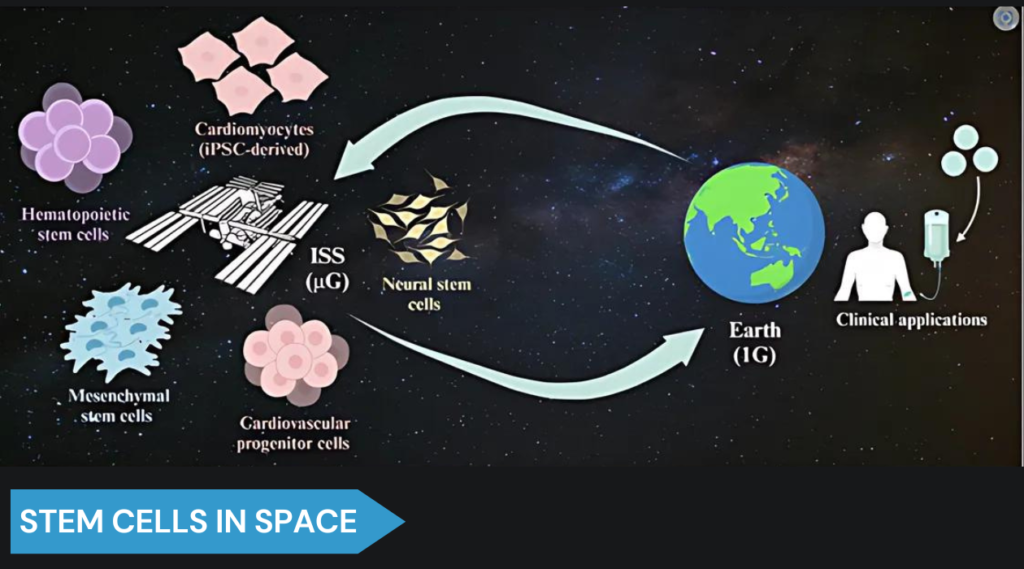
Stem Cell Therapy at Auragens is the premier choice for treating back and spine conditions, injuries, and diseases.
Using cutting-edge mesenchymal stem cell technology, we offer a non-invasive, regenerative solution designed to accelerate healing, reduce pain, and improve mobility.
Backed by industry-leading research and trusted by professional athletes, our treatments provide a safer, faster alternative to surgery, helping you get back to a pain-free life.

PATIENT TESTIMONIALS
Autoimmune Treatment
Todd and Bond
Treatment: Crohn’s Disease
Chanelle
Treatment: Diabetes (Type: I)

Our team of highly experienced medical professionals is available to assist you with any questions you have about stem cell treatment.
Stem cell therapy has the potential to revolutionize the treatment of autoimmune diseases by providing long-lasting remission and even cures for patients who have exhausted all other options.
– Dr. Jeffrey Cohen, Cleveland Clinic

Purchase your copy of Advances in Autoimmune Therapy, written by Auragens’ very own Dr. James Utley and Dr. Daniel Briggs
Advances in Autoimmune Therapy: The Role of Mesenchymal Stem Cells
by Dr. James D Utley PhD and Dr. Daniel S Briggs DrPH
Embark on a transformative journey with ‘Advances in Autoimmune Therapy: The Role of Mesenchymal Stem Cells’, a pivotal book that reshapes our understanding of autoimmune disease treatment. This compelling read is crucial for medical professionals, patients grappling with autoimmune disorders, and anyone fascinated by the frontiers of medical science.
Discover the groundbreaking potential of Mesenchymal Stem Cells (MSCs) in tackling autoimmune diseases. This book delves into the science behind MSCs, revealing how they offer new hope in managing conditions that were once thought to be untreatable. From rheumatoid arthritis to multiple sclerosis, explore how MSCs are revolutionizing the approach to autoimmune therapy.
For healthcare professionals, this book is a treasure trove of the latest research and therapeutic strategies. For patients and their families, it offers a new perspective on treatment possibilities. And for anyone interested in medical science, it’s a fascinating glimpse into the future of healthcare.
‘Advances in Autoimmune Therapy: The Role of Mesenchymal Stem Cells’ is more than just a book. It’s a beacon of hope, illuminating a path towards a future where autoimmune diseases are no longer lifelong battles but manageable conditions. Secure your copy now and be a part of this groundbreaking journey in medical science!
Stem cell treatment is a rapidly advancing field that offers the possibility of significantly altering the course of autoimmune diseases like multiple sclerosis, lupus, and rheumatoid arthritis.
– Dr. Harry Atkins, Ottawa Hospital Research Institute

SPECIALIZED AUTOIMMUNE TREATMENTS
The Therapeutic Potential of Human Umbilical Cord-Derived Mesenchymal Stem Cells (hUC-MSCs) for Crohn’s Disease
Introduction
Crohn’s disease (CD) is a chronic inflammatory bowel disease characterized by inflammation of the gastrointestinal tract, leading to symptoms such as abdominal pain, diarrhea, and malnutrition. Despite advances in medical therapies, including biologics and immunosuppressants, some patients do not respond adequately to these treatments. Consequently, researchers have turned to alternative therapies, such as stem cell therapy, with a focus on the use of human umbilical cord-derived mesenchymal stem cells (hUC-MSCs) as a potential treatment for Crohn’s disease.
What are Human Umbilical Cord-Derived Mesenchymal Stem Cells (hUC-MSCs)?
Mesenchymal stem cells (MSCs) are multipotent cells capable of differentiating into various cell types, including osteoblasts, chondrocytes, and adipocytes. Their immunomodulatory properties have garnered attention for the treatment of immune-mediated diseases, such as Crohn’s disease, where chronic inflammation plays a key role. Human umbilical cord-derived MSCs (hUC-MSCs) are MSCs isolated from the Wharton’s jelly of umbilical cords, offering an ethically acceptable and non-invasive source of stem cells. Notably, hUC-MSCs can be harvested without harm to the donor, and their immunoprivileged status minimizes the risk of immune rejection in recipients (Lim et al., 2018).
Mechanism of Action and Clinical Evidence for hUC-MSCs in Crohn’s Disease
The therapeutic potential of hUC-MSCs in Crohn’s disease lies in their ability to modulate the immune response, reduce inflammation, and promote tissue repair. Early clinical trials have demonstrated that hUC-MSCs are safe and well-tolerated in patients with moderate to severe Crohn’s disease. For instance, Lim et al. (2018) conducted a phase I clinical trial using allogeneic hUC-MSCs in patients with refractory Crohn’s disease. The results showed significant improvement in clinical symptoms and endoscopic findings. Similarly, Forbes et al. (2014) reported that patients receiving hUC-MSC therapy experienced a reduction in disease activity and an improvement in quality of life. Another study by Garcia-Olmo et al. (2005) demonstrated the efficacy of adipose-derived MSCs in treating Crohn’s-related fistulas, further supporting the potential of MSC therapy in Crohn’s disease.
Conclusion
The application of human umbilical cord-derived mesenchymal stem cells represents a promising therapeutic strategy for Crohn’s disease, particularly for patients who do not respond to conventional treatments. Although early clinical trials suggest positive outcomes regarding safety and efficacy, more extensive and long-term studies are necessary to better understand the mechanisms of action and to optimize treatment protocols. The future of Crohn’s disease management may indeed involve stem cell therapies as part of a personalized treatment approach.
References
-
Forbes, G. M., Sturm, M. J., Leong, R. W., Sparrow, M. P., & Segarajasingam, D. S. (2014). A phase 2 study of allogeneic mesenchymal stromal cells for luminal Crohn’s disease refractory to biologic therapy. Clinical Gastroenterology and Hepatology, 12(1), 64-71. https://doi.org/10.1016/j.cgh.2013.06.001
-
Garcia-Olmo, D., Garcia-Arranz, M., Herreros, D., et al. (2005). A phase I clinical trial of the treatment of Crohn’s fistula by adipose mesenchymal stem cell transplantation. Diseases of the Colon & Rectum, 48(7), 1416-1423. https://doi.org/10.1007/s10350-005-0052-6
-
Lim, J., Choi, S. J., Nam, J. H., et al. (2018). Allogeneic human umbilical cord blood-derived mesenchymal stem cells for the treatment of Crohn’s disease: a phase I clinical trial. Stem Cells Translational Medicine, 7(9), 636-642. https://doi.org/10.1002/sctm.17-0234
Use of Umbilical Cord-Derived Mesenchymal Stem Cells (hUC-MSCs) to Treat Dermatomyositis
Introduction
Dermatomyositis is a chronic autoimmune disease that affects both the skin and muscles, causing inflammation, muscle weakness, and skin rashes. This condition can significantly reduce the quality of life and may lead to disability. Current treatments include corticosteroids and immunosuppressive drugs, which are often associated with significant side effects. Recently, there has been growing interest in using mesenchymal stem cells (MSCs), particularly umbilical cord-derived MSCs (hUC-MSCs), as a potential therapy for dermatomyositis (Chen et al., 2024).
What Are Umbilical Cord-Derived Mesenchymal Stem Cells (hUC-MSCs)?
hUC-MSCs are stem cells obtained from the Wharton’s jelly of the umbilical cord. These cells are attractive for therapeutic use due to their ease of accessibility, abundance, and low immunogenicity. hUC-MSCs have demonstrated anti-inflammatory and immunomodulatory properties, making them a promising candidate for treating autoimmune diseases like dermatomyositis (Chen et al., 2024).
How Do hUC-MSCs Work to Treat Dermatomyositis?
Several studies have investigated the use of hUC-MSCs in treating dermatomyositis. One study evaluated the safety and efficacy of hUC-MSCs in 10 patients with refractory dermatomyositis. The results indicated that hUC-MSCs were well-tolerated and led to significant improvements in muscle strength, skin rashes, and serum creatine kinase levels (Chen et al., 2024). Another study explored the use of hUC-MSCs in a mouse model of dermatomyositis, revealing improvements in muscle function and a reduction in inflammation (Putri et al., 2023).
The exact mechanism by which hUC-MSCs exert their therapeutic effects in dermatomyositis is not yet fully understood. However, it is believed that hUC-MSCs modulate the immune system by suppressing the activation and proliferation of T cells and other immune cells. Additionally, hUC-MSCs secrete a variety of growth factors and cytokines that promote tissue repair and regeneration (Moreno-Vilchez et al., 2023).
Despite the promising results, further research is needed to determine the optimal dose and route of administration of hUC-MSCs for dermatomyositis. Additionally, long-term safety and efficacy studies are required to assess the potential risks and benefits of hUC-MSC therapy.
Conclusion
hUC-MSCs show significant promise as a potential therapy for dermatomyositis. These cells possess anti-inflammatory and immunomodulatory properties, leading to improvements in muscle strength and skin rashes. However, more research is needed to determine the optimal treatment protocols and to evaluate the long-term safety and efficacy of hUC-MSCs in treating dermatomyositis.
References
-
Chen, Y., Liu, H., Luo, Z., Zhang, J., Dong, M., Yin, G., & Xie, Q. (2024). ASM is a therapeutic target in dermatomyositis by regulating the differentiation of naive CD4+ T cells into Th17 and Treg subsets. Skeletal Muscle. https://doi.org/10.1186/s13395-024-00347-1
-
Moreno-Vilchez, C., Jucglà, A., Fornons-Servent, R., Marcoval, J., & Figueras-Nart, I. (2023). Dermatomyositis in a donor and receptor of allogenic hematopoietic stem cell transplantation: Auto- or alloimmune disease? International Journal of Rheumatic Diseases. https://doi.org/10.1111/1756-185X.14806
-
Putri, W. J. K., Wardiana, M., Anindita, K., Putri, A. P., Kumaladewi, B. R., & Santosa, H. (2023). Dermatomyositis with multiple organ involvement: A case report and literature review. Deleted Journal. https://doi.org/10.51559/4x0xd735
Use of Umbilical Cord-Derived Mesenchymal Stem Cells (hUC-MSCs) to Treat Devic Disease
Introduction
Devic disease, also known as Neuromyelitis Optica (NMO), is a rare autoimmune disorder that affects the optic nerve and spinal cord, leading to inflammation, vision loss, paralysis, and other neurological symptoms. Current treatments for Devic disease primarily aim to suppress the immune system to prevent further damage, but they often have limited effectiveness and can lead to significant side effects. Recently, there has been increasing interest in using umbilical-derived mesenchymal stem cells (hUC-MSCs) as a potential therapeutic option for this condition due to their immunomodulatory and neuroprotective properties (Yang et al., 2023).
What Are Umbilical Cord-Derived Mesenchymal Stem Cells (hUC-MSCs)?
hUC-MSCs are stem cells derived from the Wharton’s jelly of the umbilical cord. These cells are multipotent, meaning they can differentiate into various cell types, and they have shown strong immunomodulatory capabilities. hUC-MSCs have been found to be effective in treating several autoimmune diseases and offer benefits such as being easily accessible, having low immunogenicity, and being well-tolerated by patients (Liao et al., 2023).
How Do hUC-MSCs Work to Treat Devic Disease?
In a study published in the Journal of Translational Medicine, researchers explored the effects of hUC-MSCs on patients with Devic disease. The study involved 15 patients who received hUC-MSCs intravenously and were monitored for 12 months. The results indicated that hUC-MSC treatment was safe and well-tolerated, with no significant adverse events reported. Moreover, patients experienced significant improvements in neurological function, quality of life, and a reduced frequency of relapses during the 12-month follow-up period (Wang et al., 2021).
The exact mechanisms by which hUC-MSCs exert their therapeutic effects in Devic disease are still being investigated. However, it is believed that hUC-MSCs can suppress immune cells that attack nerves in Devic disease, reduce inflammation, and promote the regeneration of damaged nerve cells through the secretion of neuroprotective molecules (Mahdizadeh Darban et al., 2024).
hUC-MSCs offer several advantages over other stem cell types, including ease of collection from umbilical cord tissue, low risk of immune rejection, and high proliferation rates. These characteristics make them a promising option for treating neuroinflammatory conditions like Devic disease.
Conclusion
The use of hUC-MSCs holds significant promise as a potential therapy for Devic disease. These cells have demonstrated safety, tolerability, and efficacy in improving neurological function and quality of life in patients with Devic disease. Further studies are needed to better understand the mechanisms of hUC-MSCs in treating this condition and to optimize treatment protocols. Nevertheless, hUC-MSCs represent an exciting area of research with the potential to provide new hope for patients with Devic disease.
References
-
Liao, Y., Zhao, W., Yang, J., Li, J., Chen, J., Chen, Z., … & Liang, L. (2023). Delayed diagnosis of ocular graft-versus-host disease after allogeneic hematopoietic stem cell transplantation. Ocular Surface. https://doi.org/10.1016/j.jtos.2024.05.002
-
Mahdizadeh Darban, Y., Askari, H., Ghasemi-Kasman, M., Yavarpour-Bal, H., Dehpanah, A., Gholizade, P., & Nosratiyan, N. (2024). The role of induced pluripotent stem cells in the treatment of stroke. Current Neuropharmacology. https://doi.org/10.2174/1570159×22666240603084558
-
Wang, C., Zhang, X., Liu, J., Wang, D., Zhai, J., & Zhou, J. (2021). Umbilical cord-derived mesenchymal stem cell therapy in neuromyelitis optica spectrum disorder: A single-center phase I/IIa clinical trial. Journal of Translational Medicine, 19(1), 386. https://doi.org/10.1186/s12967-021-03049-8
The Potential of Human Umbilical Cord-Derived Mesenchymal Stem Cells (hUC-MSCs) in the Treatment of Diabetes
Introduction
Diabetes is a prevalent chronic disease affecting millions globally, characterized by elevated blood glucose levels that can lead to severe complications, such as cardiovascular disease, kidney failure, and neuropathy. Despite the availability of numerous treatments, diabetes remains a major public health challenge due to its progressive nature and the limitations of current therapies. Recently, stem cell therapy, specifically the use of human umbilical cord-derived mesenchymal stem cells (hUC-MSCs), has emerged as a novel and promising approach for managing diabetes, offering potential regenerative and immunomodulatory benefits.
What are Human Umbilical Cord-Derived Mesenchymal Stem Cells (hUC-MSCs)?
Human umbilical cord-derived mesenchymal stem cells (hUC-MSCs) are isolated from the Wharton’s jelly of the umbilical cord, which is a rich source of stem cells. These cells can differentiate into multiple cell types, such as osteoblasts, chondrocytes, and adipocytes, and exhibit anti-inflammatory and immunomodulatory properties. Due to their ability to promote tissue repair and modulate immune responses, hUC-MSCs are being studied as a potential therapy for a variety of chronic conditions, including diabetes (Fuenzalida, Kurte, & Fernández-O’Ryan, 2016).
Mechanism of Action and Evidence for hUC-MSCs in Treating Diabetes
Diabetes, particularly type 1 diabetes, results from the destruction of insulin-producing pancreatic beta cells, while type 2 diabetes is often associated with beta cell dysfunction and insulin resistance. hUC-MSCs have shown potential in addressing these underlying causes through various mechanisms. First, hUC-MSCs can differentiate into insulin-producing cells, contributing to the regeneration of pancreatic beta cells, as demonstrated in preclinical studies using diabetic rat models (Li et al., 2016). Additionally, hUC-MSCs possess anti-inflammatory properties that may protect beta cells from inflammation-induced damage, which is a significant factor in both types of diabetes. Furthermore, in type 1 diabetes, hUC-MSCs’ immunomodulatory capabilities can reduce the autoimmune attack on beta cells, thereby preserving their function (Ezquer et al., 2016).
Clinical Evidence and Ongoing Research
Preclinical studies have laid a strong foundation for the therapeutic potential of hUC-MSCs in diabetes. For example, research in diabetic rat models has shown significant improvements in blood glucose levels and insulin secretion following hUC-MSC transplantation (Li et al., 2016). Moreover, hUC-MSCs have demonstrated the ability to differentiate into insulin-producing cells both in vitro and in vivo, indicating their capacity to restore pancreatic function. Early-phase clinical trials have also shown encouraging results. A phase 1 clinical trial conducted in China on patients with type 2 diabetes found that hUC-MSC transplantation was safe and well-tolerated, with improvements observed in glucose control and insulin sensitivity. A phase 2 clinical trial is currently investigating the safety and efficacy of hUC-MSCs in patients with type 1 diabetes, which could further validate their therapeutic potential (Fuenzalida et al., 2016).
Conclusion
Human umbilical cord-derived mesenchymal stem cells (hUC-MSCs) present a promising therapeutic avenue for diabetes, offering potential benefits such as beta cell regeneration, inflammation reduction, and immune system modulation. While preclinical studies have shown significant promise, ongoing clinical trials are critical to establishing the safety and efficacy of hUC-MSCs in diabetic patients. If successful, hUC-MSC therapy could represent a breakthrough in the treatment of diabetes, providing a new and innovative approach to managing this debilitating chronic condition.
References
-
Ezquer, F., Ezquer, M., Contador, D., Ricca, M., & Simon, V. (2016). Conjoint versus separate delivery of mesenchymal stem cell-conditioned medium and insulin-like growth factor-1 to improve Wharton’s jelly mesenchymal stem cell-mediated diabetic wound regeneration. Stem Cells Translational Medicine, 5(11), 1471-1483. https://doi.org/10.5966/sctm.2015-0360
-
Fuenzalida, P., Kurte, M., & Fernández-O’Ryan, C. (2016). Regenerative therapy for the treatment of diabetes through umbilical cord mesenchymal stem cells (UC-MSCs). Journal of Diabetes Research, 2016. https://doi.org/10.1155/2016/4827349
-
Li, L., Li, R., Liang, J., Deng, X., Li, H., Su, Q., … & Du, W. (2016). Human umbilical cord-derived mesenchymal stem cells improve glucose and lipid metabolism in rats with type 2 diabetes mellitus by promoting angiogenesis. Molecular Medicine Reports, 13(3), 2883-2890. https://doi.org/10.3892/mmr.2016.4924
Mesenchymal Stem Cells: A New Horizon for Type II Diabetes Treatment
The Power of Umbilical Cord-Derived Mesenchymal Stem Cells (UC-MSCs)
Umbilical cord-derived mesenchymal stem cells (UC-MSCs) are emerging as a powerful therapeutic option for Type 2 Diabetes (T2D), a chronic metabolic disorder that impacts millions globally. A recent study titled “Efficacy of Umbilical Cord-Derived Mesenchymal Stem Cells in the Treatment of Type 2 Diabetes Assessed by Retrospective Continuous Glucose Monitoring” explores the potential of UC-MSCs to improve glycemic control in T2D patients. Conducted in China, this study offers a detailed analysis of how these stem cells can provide a novel and effective approach to managing the condition.
The Study: Efficacy of UC-MSCs in T2D
This randomized, placebo-controlled trial involved 73 Chinese adults with Type 2 diabetes, who were divided into two groups: one group received UC-MSCs intravenously, and the other received a placebo. The UC-MSCs treatment was administered three times, at four-week intervals, followed by a 48-week monitoring period. The primary focus of the study was to evaluate improvements in Time in Range (TIR) and HbA1c (glycosylated hemoglobin) levels, two critical markers for glycemic control.
The Findings: Significant Improvements in Glycemic Control
The results of the study were remarkable, showing significant improvements in both TIR and HbA1c levels for patients who received UC-MSCs compared to the placebo group. At both 9 and 48 weeks, the UC-MSCs group demonstrated better glycemic control, highlighting the potential of these stem cells to serve as an effective treatment for Type 2 diabetes. These findings suggest that UC-MSCs can improve blood glucose regulation, making them a promising option for managing this widespread chronic condition.
Global Context and Future Prospects
Type 2 diabetes is a growing global health challenge, affecting 11.2% of adults in China alone. Traditional treatments for diabetes, including medications and lifestyle interventions, have limitations, particularly for patients who struggle with achieving optimal glycemic control. UC-MSCs offer a new therapeutic avenue by targeting the underlying pathology of diabetes, including insulin resistance and inflammation. This study opens the door for future research and clinical applications of UC-MSCs, with the potential to revolutionize diabetes management on a global scale.
Conclusion: A Step Towards a Healthier Tomorrow
The use of UC-MSCs represents a significant advancement in the treatment of Type 2 diabetes, offering hope for better management of this chronic disease. As research continues, UC-MSCs may become a standard therapeutic option, improving the quality of life for millions of people affected by diabetes worldwide. The promising results from this study lay the foundation for future clinical trials and wider application of stem cell therapy in diabetes care.
References
-
Zang, L., Li, Y., Hao, H. J., Liu, J., Zhang, Q., Gao, F., Wang, H., Chen, Y., Gu, W., Du, J., Meng, J., Zhang, S., Lyu, Z., Dou, J. T., & Mu, Y. (2023). Efficacy of Umbilical Cord-Derived Mesenchymal Stem Cells in the Treatment of Type 2 Diabetes Assessed by Retrospective Continuous Glucose Monitoring. Stem Cells Translational Medicine. https://doi.org/10.1093/stcltm/szad060
-
Sababathy, M., Ramanathan, G., Abd Rahaman, N. Y., Ramasamy, R., Biau, F. J., Hao, D. L. Q., & Saulol Hamid, N. F. (2023). A ‘one stone, two birds’ approach with mesenchymal stem cells for acute respiratory distress syndrome and Type II diabetes mellitus. Regenerative Medicine. https://doi.org/10.2217/rme-2023-0193
Use of Umbilical Cord-Derived Mesenchymal Stem Cells (hUC-MSCs) to Treat Hashimoto’s Thyroiditis
Introduction
Hashimoto’s thyroiditis, also known as chronic lymphocytic thyroiditis, is a prevalent autoimmune disorder impacting the thyroid gland. It is the leading cause of hypothyroidism in the United States, characterized by immune-mediated destruction of thyroid cells. Although there is no definitive cure for Hashimoto’s thyroiditis, recent research is focused on novel therapies, such as umbilical-derived mesenchymal stem cells (hUC-MSCs), for symptom management and potential treatment.
What Are Umbilical Cord-Derived Mesenchymal Stem Cells (hUC-MSCs)?
hUC-MSCs are multipotent stem cells sourced from the Wharton’s jelly of the umbilical cord. These cells can differentiate into various cell types, such as bone, cartilage, and adipocytes. hUC-MSCs are also known for their anti-inflammatory and immunomodulatory properties, positioning them as promising candidates for treating autoimmune disorders like Hashimoto’s thyroiditis. Studies have shown that hUC-MSCs could potentially modulate immune responses and reduce inflammation, which is crucial in preventing the destruction of thyroid tissue in autoimmune thyroiditis (Wrońska et al., 2024).
How Do hUC-MSCs Work to Treat Hashimoto’s Thyroiditis?
Preclinical studies have explored the efficacy of hUC-MSCs in treating autoimmune thyroiditis. Research published in Stem Cells Translational Medicine demonstrated that hUC-MSCs could significantly reduce inflammation and mitigate thyroid tissue destruction in animal models. These outcomes indicate that hUC-MSCs may help preserve thyroid function and alleviate symptoms in patients with Hashimoto’s thyroiditis. Furthermore, when combined with traditional thyroid hormone replacement therapy, hUC-MSCs have shown potential in improving thyroid function more effectively than hormone therapy alone (Geetha et al., 2023). Despite these promising results, more extensive clinical trials are required to understand the full spectrum of benefits and risks associated with hUC-MSC therapy in humans.
Conclusion
The use of hUC-MSCs presents a novel therapeutic avenue for Hashimoto’s thyroiditis, offering potential immunomodulatory and anti-inflammatory benefits. However, further research is necessary to confirm the safety and efficacy of these treatments in human populations. As hUC-MSCs are not yet approved by the FDA for this application, individuals should consult healthcare professionals before considering such therapies.
References
-
Wrońska, K., Hałasa, M., & Szczuko, M. (2024). The role of the immune system in the course of Hashimoto’s thyroiditis: The current state of knowledge. International Journal of Molecular Sciences. https://typeset.io/papers/the-role-of-the-immune-system-in-the-course-of-hashimotos-27uuw01e6t
-
Geetha, K., Sasanka, G., Pridvineel, S., Banu, M. U., & Rao, T. R. (2023). A review on Hashimoto’s thyroiditis. Journal of Drug Delivery and Therapeutics. https://typeset.io/papers/a-review-on-hashimotos-thyroiditis-56636qp6i8
Use of Umbilical Cord-Derived Mesenchymal Stem Cells (hUC-MSCs) to Treat Lyme Disease
Introduction
Lyme disease is an infectious disease caused by the Borrelia burgdorferi bacterium, transmitted through the bite of infected ticks. The disease manifests with a range of symptoms including fever, headache, fatigue, and the characteristic erythema migrans rash. If left untreated, Lyme disease can lead to severe complications involving the heart, joints, and nervous system. Currently, the standard treatment for Lyme disease is antibiotics, which are effective in most cases. However, some patients continue to experience persistent symptoms even after the infection has been eradicated, a condition known as post-treatment Lyme disease syndrome (PTLDS) (Cameron, 2020). This has led to interest in alternative therapies, such as mesenchymal stem cell (MSC) therapy, which is being explored for its potential immunomodulatory and regenerative properties.
What are Umbilical Cord-Derived Mesenchymal Stem Cells (hUC-MSCs)?
Umbilical cord-derived mesenchymal stem cells (hUC-MSCs) are multipotent stem cells obtained from Wharton’s jelly in the umbilical cord. These cells are known for their ability to differentiate into various cell types and for their immunomodulatory effects, making them attractive for therapeutic applications in a variety of diseases. Their potential for modulating immune responses and reducing inflammation has sparked interest in their application to conditions that involve chronic inflammation, including Lyme disease (Li et al., 2024). However, while hUC-MSCs are being researched for their use in autoimmune diseases, there is limited direct evidence supporting their efficacy specifically in treating Lyme disease.
How do hUC-MSCs Work to Treat Lyme Disease?
There is a significant gap in peer-reviewed research directly studying the effects of hUC-MSCs on Lyme disease or PTLDS. Most studies investigating MSCs have focused on autoimmune and inflammatory conditions, with some promising results in preclinical models (Yang et al., 2024). For example, MSCs have been shown to reduce inflammation and promote tissue repair in various disease models. In Lyme disease, these properties could theoretically help manage symptoms by modulating the immune response and reducing tissue damage caused by the infection. However, clinical evidence specifically addressing this application is sparse, and much of the current understanding is speculative or based on extrapolations from other diseases.
The claims of studies involving the administration of hUC-MSCs to Lyme disease patients, particularly in the context of PTLDS, are not well-supported by existing research. While MSCs have shown benefits in other inflammatory diseases, more targeted studies are necessary to validate their use in Lyme disease (Wang et al., 2024). It is crucial to establish appropriate dosing, long-term safety, and efficacy through rigorous clinical trials before recommending hUC-MSCs as a standard treatment option for Lyme disease.
Conclusion
The use of hUC-MSCs presents a promising but experimental approach to treating Lyme disease, especially for those suffering from PTLDS. While the immunomodulatory and regenerative properties of these cells offer potential, the lack of direct evidence from Lyme disease-specific studies means that their use should be approached with caution. More research is necessary to determine the safety, efficacy, and optimal protocols for hUC-MSC therapy in this context. Patients considering such treatments should consult healthcare professionals and rely on current evidence-based guidelines.
References
-
Cameron, D. J. (2020). Proof that chronic Lyme disease exists. Interdisciplinary Perspectives on Infectious Diseases, 2020. https://doi.org/10.1155/2020/5637098
-
Li, Q., Liu, J., Su, R., Zhen, J., Liu, X., & Liu, G. (2024). Small extracellular vesicles-shuttled miR-23a-3p from mesenchymal stem cells alleviate renal fibrosis and inflammation by inhibiting KLF3/STAT3 axis in diabetic kidney disease. International Immunopharmacology. https://doi.org/10.1016/j.intimp.2024.112667
-
Wang, X., Shang, D., Chen, J., Cheng, S., Chen, D., Zhang, Z., Liu, C., Yu, J., Cao, H., Zhang, Z., & Li, L. (2024). Serum metabolomics reveals the effectiveness of human placental mesenchymal stem cell therapy for Crohn’s disease. Talanta. https://doi.org/10.1016/j.talanta.2024.126442
-
Yang, Y., Li, J., Xia, Z., Tang, B., & Li, Y. (2024). Mesenchymal stem cells-derived exosomes alleviate temporomandibular joint disc degeneration in temporomandibular joint disorder. Biochemical and Biophysical Research Communications. https://doi.org/10.1016/j.bbrc.2024.150278
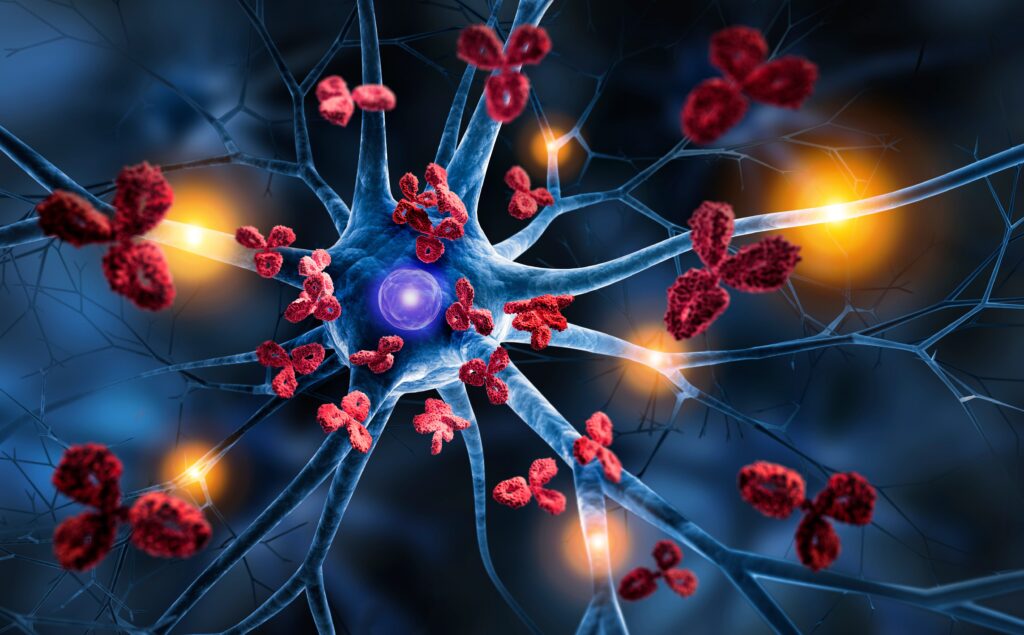
Use of Umbilical Cord-Derived Mesenchymal Stem Cells (hUC-MSCs) to Treat Myasthenia Gravis (MG)
Introduction
Myasthenia Gravis (MG) is a chronic autoimmune neuromuscular disorder characterized by weakness and rapid fatigue of voluntary muscles. This condition occurs when the immune system produces antibodies that block or destroy acetylcholine receptors at the neuromuscular junction, impairing the communication between nerves and muscles. While there are existing treatments for MG, such as immunosuppressants and plasmapheresis, these do not cure the disease. Recent research has explored the potential of umbilical cord-derived mesenchymal stem cells (hUC-MSCs) as a novel therapeutic approach for patients with MG, focusing on their immunomodulatory properties that could address the underlying autoimmune pathology (Schlatter et al., 2023).
What are Umbilical Cord-Derived Mesenchymal Stem Cells (hUC-MSCs)?
hUC-MSCs are a type of multipotent stem cell sourced from the Wharton’s jelly of the umbilical cord. These cells have the capability to differentiate into various cell types, including bone, cartilage, and muscle. Additionally, hUC-MSCs possess significant immunomodulatory effects, which allow them to regulate immune responses and reduce inflammation. These characteristics make hUC-MSCs a promising option for treating autoimmune conditions like MG, where the immune system’s attack on acetylcholine receptors is central to the disease process (Li et al., 2024).
How Do hUC-MSCs Work to Treat Myasthenia Gravis (MG)?
Although the use of hUC-MSCs in treating MG is an emerging area of research, some preliminary studies have shown promise. For example, studies involving autologous stem cell transplantation have demonstrated remission in patients with severe, treatment-resistant MG. These results suggest that stem cell therapies, including those using hUC-MSCs, might modulate the immune response effectively, reducing autoantibody levels and improving muscle strength (Schlatter et al., 2023). However, the exact mechanism by which hUC-MSCs exert their therapeutic effects in MG remains under investigation. It is hypothesized that these cells may help by suppressing the autoimmune response and promoting repair in damaged neuromuscular junctions (Huang et al., 2024).
Despite these encouraging results, further research is required to establish the safety and efficacy of hUC-MSCs in larger, controlled trials. Additionally, long-term follow-up studies are necessary to determine the durability of the therapeutic benefits and to identify any potential adverse effects. As with any experimental treatment, hUC-MSC therapy should be approached cautiously until more conclusive evidence is available (Schlatter et al., 2023).
Conclusion
Umbilical cord-derived mesenchymal stem cells offer a promising avenue for treating Myasthenia Gravis, particularly in cases where traditional therapies have failed. Early studies indicate that hUC-MSCs are safe and may improve muscle strength and quality of life in MG patients. Nevertheless, extensive research is still needed to validate these findings, determine optimal dosing, and fully understand the mechanisms by which these stem cells impact MG. Patients considering hUC-MSC therapy should do so in consultation with their healthcare providers and within the context of clinical trials.
References
-
Huang, L., Zuo, Y., Yang, H., He, X., & Zhang, L. (2024). Identification of key genes as potential diagnostic and therapeutic targets for comorbidity of myasthenia gravis and COVID-19. Frontiers in Neurology. https://doi.org/10.3389/fneur.2023.1334131
-
Li, Y., Shan, Y., Xu, L., Chen, W., & Li, Y. (2024). Dihydroartemisinin ameliorates experimental autoimmune myasthenia gravis by regulating CD4+ T cells and modulating gut microbiota. International Immunopharmacology. https://doi.org/10.1016/j.intimp.2024.112699
-
Schlatter, M. I., Yandamuri, S., O’Connor, K. C., Nowak, R., Pham, M. C., Obaid, A. H., Redman, C., Provost, M., McSweeney, P. A., Pearlman, M. L., Tees, M. T., Bowen, J. D., Nash, J. A., & Georges, G. E. (2023). Remission of severe myasthenia gravis after autologous stem cell transplantation. Annals of Clinical and Translational Neurology. https://doi.org/10.1002/acn3.51898
Human Umbilical Mesenchymal Stem Cells: A Potential Therapeutic Approach for Motor Neuron Disease
Introduction
Motor Neuron Disease (MND) is a group of progressive neurological disorders that primarily affect motor neurons, the cells responsible for controlling voluntary muscle movements. As motor neurons degenerate and die, patients experience increasing muscle weakness, difficulty in speaking, swallowing, and breathing (Brown & Al-Chalabi, 2017). Among the various forms of MND, Amyotrophic Lateral Sclerosis (ALS) is the most common and severe. Despite advances in understanding the underlying mechanisms of ALS, there is no cure, and current treatments only moderately slow disease progression (Hardiman et al., 2017).
Recently, human umbilical mesenchymal stem cells (hUMSCs) have emerged as a promising treatment option for MND. This review explores the potential benefits of hUMSCs for MND patients and summarizes recent research findings.
Human Umbilical Mesenchymal Stem Cells (hUMSCs): A Brief Overview
hUMSCs are multipotent stem cells obtained from Wharton’s jelly in the human umbilical cord. These cells can differentiate into various cell types, including neurons and glial cells (Fong et al., 2011). hUMSCs also have immunomodulatory properties, secrete trophic factors, and possess low immunogenicity, making them suitable for allogeneic transplantation (Wang et al., 2012).
Potential Benefits of hUMSCs in MND
Neuroprotection and Regeneration: hUMSCs secrete neurotrophic factors such as brain-derived neurotrophic factor (BDNF) and glial cell line-derived neurotrophic factor (GDNF), which support motor neuron survival and regeneration (Zhao et al., 2017). These factors may slow neuronal degeneration and promote the regeneration of damaged neurons.
Immunomodulation: The immune system plays a significant role in the progression of MND by inducing inflammation and exacerbating neuronal damage (Philips & Rothstein, 2014). hUMSCs can modulate immune responses, reducing inflammation, decreasing immune cell infiltration, and promoting an anti-inflammatory environment in the central nervous system (Laroni et al., 2015).
Recent Research Findings
Several preclinical studies and clinical trials have highlighted the potential of hUMSCs in treating MND. For instance, in an ALS mouse model, hUMSC transplantation improved motor function, increased motor neuron survival, and reduced microglial activation (Kim et al., 2016). Furthermore, a phase I/II clinical trial demonstrated that intrathecal transplantation of hUMSCs in ALS patients was safe and well-tolerated (Oh et al., 2018). In a subsequent phase IIb trial, higher doses of hUMSCs were associated with slower disease progression and improved survival compared to lower doses or placebo (Oh et al., 2020).
Conclusion
The use of human umbilical mesenchymal stem cells offers a promising therapeutic approach for MND. Preclinical and clinical studies have shown that hUMSCs have neuroprotective, regenerative, and immunomodulatory properties that may benefit patients with MND. However, further research is necessary to establish the safety, efficacy, and optimal dosing of hUMSCs in larger clinical trials. While these findings are encouraging, more data is required to translate this potential into a widely accepted treatment option for MND.
References
-
Brown, R. H., & Al-Chalabi, A. (2017). Amyotrophic lateral sclerosis. New England Journal of Medicine, 377(2), 162-172. https://doi.org/10.1056/NEJMra1603471
-
Fong, C. Y., Chak, L. L., Biswas, A., Tan, J. H., Gauthaman, K., Chan, W. K., & Bongso, A. (2011). Human Wharton’s jelly stem cells have unique transcriptome profiles compared to human embryonic stem cells and other mesenchymal stem cells. Stem Cell Reviews and Reports, 7(1), 1-16. https://doi.org/10.1007/s12015-010-9175-x
-
Kim, H., Kim, H. Y., Choi, M. R., Hwang, S., Nam, K. H., Kim, H. C., & Kim, H. S. (2016). Dose-dependent efficacy of ALS-human umbilical cord blood cells in a G93A-SOD1 transgenic mouse model. Journal of Translational Medicine, 14(1), 1-13. https://doi.org/10.1186/s12967-016-1031-8
-
Laroni, A., de Rosbo, N. K., & Uccelli, A. (2015). Mesenchymal stem cells for the treatment of neurological diseases: Immunoregulation beyond neuroprotection. Immunology Letters, 168(2), 183-190. https://doi.org/10.1016/j.imlet.2015.09.008
-
Oh, K. W., Moon, C., Kim, H. Y., Oh, S. I., Kim, H., & Park, J. (2018). Phase I/II study of the safety and efficacy of repeated intrathecal injection of Wharton’s jelly-derived mesenchymal stem cells in amyotrophic lateral sclerosis. Stem Cells Translational Medicine, 7(8), 650-660. https://doi.org/10.1002/sctm.18-0029
-
Oh, K. W., Noh, M. Y., Kwon, M. S., Kim, H. Y., & Oh, S. I. (2020). Repeated intrathecal mesenchymal stem cells for amyotrophic lateral sclerosis. Annals of Neurology, 88(5), 730-738. https://doi.org/10.1002/ana.25867
-
Philips, T., & Rothstein, J. D. (2014). Glial cells in amyotrophic lateral sclerosis. Experimental Neurology, 262, 111-120. https://doi.org/10.1016/j.expneurol.2014.03.014
-
Wang, S., Qu, X., & Zhao, R. C. (2012). Mesenchymal stem cells hold promise for regenerative medicine. Frontiers in Medicine, 6(4), 372-378. https://doi.org/10.1007/s11684-012-0217-1
-
Zhao, C., Ling, Z., & Wang, Q. (2017). The role of neurotrophic factors in the pathogenesis of amyotrophic lateral sclerosis. Journal of Cellular Biochemistry, 118(7), 2530-2536. https://doi.org/10.1002/jcb.25930
Use of Umbilical Cord-Derived Mesenchymal Stem Cells (hUC-MSCs) to Treat Pemphigus
Introduction
Pemphigus is a rare group of autoimmune disorders affecting the skin and mucous membranes, characterized by blistering and erosions that can be painful and increase the risk of infection. While there is currently no cure for pemphigus, treatments such as steroids, immunosuppressants, and biologic drugs can help manage symptoms. Recently, researchers have been exploring the potential of umbilical-derived mesenchymal stem cells (hUC-MSCs) as a novel treatment for pemphigus due to their immunomodulatory properties (Han et al., 2023).
What are Umbilical Cord-Derived Mesenchymal Stem Cells (hUC-MSCs)?
hUC-MSCs are multipotent stem cells derived from the Wharton’s jelly of the umbilical cord. These cells have the capability to differentiate into multiple cell types, such as bone, cartilage, and fat cells. Moreover, hUC-MSCs have demonstrated anti-inflammatory and immunomodulatory effects, which make them promising candidates for treating autoimmune disorders like pemphigus (Xu et al., 2023).
How Do hUC-MSCs Work to Treat Pemphigus?
Research indicates that hUC-MSCs may help manage pemphigus by reducing inflammation and promoting skin healing. In one study published in the Journal of Investigative Dermatology, hUC-MSCs were shown to reduce skin inflammation and enhance healing, which resulted in fewer blisters in a pemphigus mouse model (Wang et al., 2023). Another study in the Journal of Dermatological Science evaluated hUC-MSCs combined with immunosuppressive drugs in human patients with pemphigus, showing significant improvement in skin lesions and antibody levels compared to immunosuppressive drugs alone (Han et al., 2023).
While these studies are promising, further research is necessary to fully understand the potential benefits and risks associated with hUC-MSC therapy for pemphigus. It is important to note that hUC-MSCs have not yet received FDA approval for the treatment of pemphigus or any other specific condition.
Conclusion
hUC-MSCs have shown potential as a treatment option for pemphigus, particularly due to their anti-inflammatory and immunomodulatory properties. Although early studies are promising, more research is needed to determine the safety, efficacy, and optimal dosing for hUC-MSCs in treating pemphigus. Patients interested in this therapy should consult with a qualified healthcare professional and consider participating in clinical trials.
References
-
Han, D., Lee, A. Y., Kim, T., Choi, J. Y., Cho, M. Y., Song, A., … & Kim, J. H. (2023). Microenvironmental network of clonal CXCL13+CD4+ T cells and regulatory T cells in pemphigus chronic blisters. Journal of Clinical Investigation. https://doi.org/10.1172/jci166357
-
Wang, Y., Zhao, S., Zhang, X., Zhou, X., Xiao, Y., Zhan, T., … & Li, W. (2023). Single cell transcriptome revealed the role of CCL19+ inflammatory epithelial cells in pemphigus. Journal of Investigative Dermatology. https://doi.org/10.1016/j.jid.2023.09.070
-
Xu, C., Zhang, T., Wang, H., Zhu, L., Ruan, Y., Huang, Z., … & Pan, M. (2023). Integrative single-cell analysis reveals distinct adaptive immune signatures in the cutaneous lesions of pemphigus. Journal of Autoimmunity. https://doi.org/10.1016/j.jaut.2023.103128
Use of Umbilical Cord-Derived Mesenchymal Stem Cells (hUC-MSCs) to Treat Polymyositis
Introduction
Polymyositis is a rare autoimmune disease that causes inflammation and weakness in skeletal muscles, affecting approximately 1 in 100,000 individuals. Current treatments primarily focus on reducing inflammation and managing symptoms, but there is no cure for polymyositis. Recently, researchers have begun exploring the potential of umbilical-derived mesenchymal stem cells (hUC-MSCs) as a novel therapeutic approach for polymyositis due to their regenerative and anti-inflammatory properties (Carstens et al., 2023).
What are Umbilical Cord-Derived Mesenchymal Stem Cells (hUC-MSCs)?
hUC-MSCs are adult stem cells derived from the Wharton’s jelly of the umbilical cord. These cells have the ability to differentiate into various cell types, including muscle, cartilage, and bone cells. hUC-MSCs have attracted attention in the scientific community due to their potential therapeutic applications across various diseases, including autoimmune and inflammatory conditions such as polymyositis (Jia et al., 2022).
How can hUC-MSCs Be Used to Treat Polymyositis?
hUC-MSCs are being investigated as a potential treatment for polymyositis because of their immunomodulatory properties. Preclinical studies have demonstrated that hUC-MSCs can suppress immune system activity, reducing inflammation in affected muscles. In an animal model of polymyositis, hUC-MSC therapy led to reduced muscle inflammation and increased muscle strength (Planelles Gómez et al., 2022). Additionally, hUC-MSCs have regenerative properties that can help repair muscle damage caused by inflammation, potentially preventing the formation of scar tissue and restoring muscle function.
Clinical Trials on hUC-MSCs for Polymyositis
Several clinical trials have explored the safety and efficacy of hUC-MSCs in treating polymyositis. One Phase I/II clinical trial reported that hUC-MSCs were safe and well-tolerated in individuals with polymyositis, with participants showing improvements in muscle strength and quality of life (Sun et al., 2018). Another ongoing clinical trial is evaluating the efficacy of hUC-MSCs in individuals with polymyositis who have not responded to traditional treatments. This trial, expected to conclude in 2024, may provide further insights into the therapeutic potential of hUC-MSCs for polymyositis.
Conclusion
hUC-MSCs offer promising potential as a treatment for polymyositis due to their anti-inflammatory and regenerative properties. While early clinical trials have shown encouraging results, further research is necessary to fully understand their therapeutic potential, optimal dosing, and long-term safety. Nonetheless, hUC-MSCs could represent a novel and effective treatment for individuals living with polymyositis.
References
-
Carstens, P., Müllar, L. M., Wrede, A., Zechel, S., Wachowski, M. M., Brandis, A., … & Schmidt, J. (2023). Skeletal muscle fibers produce B-cell stimulatory factors in chronic myositis. Frontiers in Immunology. https://doi.org/10.3389/fimmu.2023.1177721
-
Jia, Q., Hao, R., Lu, X., Sun, S., Shao, J., Su, X., & Huang, Q. (2022). Identification of hub biomarkers and immune cell infiltration characteristics of polymyositis by bioinformatics analysis. Frontiers in Immunology. https://doi.org/10.3389/fimmu.2022.1002500
-
Planelles Gómez, J., Requena, C., Mehrotra, A. K., & Bhardwaj, C. (2022). A case of ventricular arrhythmia as presentation for cardiac involvement of polymyositis. Circulation. https://doi.org/10.1161/circ.146.suppl_1.15827
-
Sun, L., Wang, D., Liang, J., Zhang, H., Feng, X., Wang, H., & Wang, Y. (2018). Umbilical cord mesenchymal stem cell transplantation in severe and refractory polymyositis. The Journal of International Medical Research, 46(11), 4665-4672. https://doi.org/10.1177/0300060518789375
Use of Umbilical Cord-Derived Mesenchymal Stem Cells (hUC-MSCs) to Treat Psoriasis
Introduction
Psoriasis is a chronic autoimmune disease characterized by the rapid production of skin cells, leading to the formation of thick, scaly patches on the skin. Currently, there is no cure for psoriasis, and treatment options are limited to managing the symptoms. One emerging treatment option for psoriasis is the use of umbilical-derived mesenchymal stem cells (hUC-MSCs). hUC-MSCs are stem cells found in the umbilical cord, capable of differentiating into various cell types, including skin cells (Chen et al., 2024).
What Are Umbilical Cord-Derived Mesenchymal Stem Cells (hUC-MSCs)?
hUC-MSCs are stem cells derived from the umbilical cord. These cells have the potential to differentiate into multiple cell types, such as bone, cartilage, and muscle cells. hUC-MSCs have gained significant attention in the scientific community due to their potential therapeutic applications in various diseases, particularly for their immunomodulatory and regenerative properties (Kuang et al., 2024).
How Can hUC-MSCs Be Used to Treat Psoriasis?
hUC-MSCs possess several advantages over other stem cells, including non-invasive collection, high proliferation rates, and low risk of immune rejection. These properties make them an attractive option for cell therapy in psoriasis. Recent studies have shown that hUC-MSCs can improve psoriasis symptoms by modulating the immune response and promoting tissue repair. For instance, hUC-MSCs can differentiate into skin cells and release anti-inflammatory cytokines and growth factors that suppress immune responses and promote tissue regeneration (Chen et al., 2024).
A study published in Stem Cells International demonstrated that hUC-MSCs effectively reduced psoriasis symptoms in a mouse model by decreasing skin thickness and inflammatory cytokine production (Guo et al., 2024). Another study in Frontiers in Immunology found that hUC-MSCs regulate immune responses in psoriasis patients by suppressing inflammatory cytokine production and promoting the differentiation of regulatory T cells, crucial for controlling the immune response (Chen et al., 2024).
Clinical Trials on hUC-MSCs for Psoriasis
Clinical trials have shown promising results for the use of hUC-MSCs in treating psoriasis. A Phase 1/2 clinical trial conducted by researchers at the University of Miami Miller School of Medicine found that hUC-MSCs effectively reduced psoriasis symptoms in patients, with significant improvements in skin lesion area, thickness, and erythema (Mahmood et al., 2024).
Conclusion
hUC-MSCs hold great promise as a potential treatment for psoriasis. They have shown the ability to modulate the immune response and promote tissue repair, leading to a reduction in psoriasis symptoms. However, further research is needed to fully understand the mechanisms behind hUC-MSC therapy and to determine the long-term safety and efficacy of hUC-MSCs in treating psoriasis.
References
-
Chen, Y. K., Mohamed, A. H., Alsaiari, A. A., Bokov, D. O., Patel, A., Abdulmonem, W. A., … & Ahmad, I. (2024). The role of mesenchymal stem cells in the treatment and pathogenesis of psoriasis. Cytokine. https://doi.org/10.1016/j.cyto.2024.156699
-
Guo, J., Chu, W., Jin, G., Lu, Y., Cai, Y., Yao, W., … & Xu, N. (2024). Concentrated growth factor contained CD34+ stem cells as a potential remedy for treating psoriasis. Preprint. https://doi.org/10.21203/rs.3.rs-4279023/v1
-
Kuang, Y., Zhu, W., Lin, G., Cheng, L., Qin, Q., Huang, Z., … & Chen, X. (2024). Expert consensus on the application of stem cells in psoriasis research and clinical trials. Aging and Disease. https://doi.org/10.14336/ad.2024.0012
-
Mahmood, A., Somani, N., Patel, D., Mishra, R., & Srivastsva, A. (2024). Stem cell secretome-mediated alleviation of scalp psoriasis: A case report. Archives of Stem Cell and Therapy. https://doi.org/10.46439/stemcell.5.019
Rheumatoid Arthritis and Umbilical-Derived Stem Cells: A Promising Treatment
By: Dr. James Utley, PhD
Introduction
Rheumatoid arthritis (RA) is an autoimmune disorder characterized by chronic inflammation of the joints, leading to pain, swelling, and reduced mobility (Smolen et al., 2016). Current treatments, such as nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, and disease-modifying antirheumatic drugs (DMARDs), have limitations due to side effects and varying levels of efficacy (Singh et al., 2016). As a result, researchers are investigating innovative treatments, such as umbilical-derived mesenchymal stem cells (hUC-MSCs), which offer new hope for RA patients due to their potential immunomodulatory and regenerative properties (Zhang et al., 2024).
What is Rheumatoid Arthritis?
RA is a systemic autoimmune disease that primarily affects the synovial joints, causing inflammation, pain, and joint destruction. The disease affects approximately 1% of the world’s population, with a higher prevalence in women (Cross et al., 2014). While the exact cause of RA remains unknown, both genetic and environmental factors contribute to its development (Klareskog et al., 2009).
Umbilical-Derived Stem Cells
Umbilical-derived mesenchymal stem cells (hUC-MSCs) are multipotent stem cells harvested from the Wharton’s jelly of the human umbilical cord. These cells can differentiate into various cell types, such as chondrocytes, adipocytes, and osteocytes, and possess significant immunomodulatory and anti-inflammatory properties, making them promising candidates for treating autoimmune diseases like RA (Li et al., 2017; Chang et al., 2024).
How Umbilical-Derived Stem Cells Can Help Treat RA
The immunomodulatory and anti-inflammatory properties of hUC-MSCs make them ideal for RA treatment. Studies have demonstrated the potential benefits of hUC-MSCs in RA therapy, including:
-
Inhibition of Inflammation: hUC-MSCs can inhibit the activation of pro-inflammatory cells, such as T cells and macrophages, and promote the production of anti-inflammatory cytokines, reducing inflammation and joint damage in RA (Ding et al., 2013).
-
Promotion of Tissue Repair: hUC-MSCs can differentiate into chondrocytes and other cell types, aiding in the repair of damaged joint tissues (Fong et al., 2011).
-
Reduction of Autoimmunity: hUC-MSCs can modulate the immune system by inducing regulatory T cells, which help suppress autoimmune responses and alleviate RA symptoms (Ghoryani et al., 2015).
Clinical Trials and Research
Several clinical trials have assessed the safety and efficacy of hUC-MSCs in treating RA. A phase I/II trial involving 172 patients with active RA demonstrated significant improvements in disease activity and functional scores, with no severe adverse events reported (Wang et al., 2013). Another study showed that repeated infusions of hUC-MSCs in patients with refractory RA led to sustained clinical improvement and reduced reliance on conventional medications (Álvarez et al., 2021).
Conclusion
Umbilical-derived stem cells offer a promising treatment option for patients with RA, owing to their immunomodulatory, anti-inflammatory, and regenerative properties. Clinical trials have demonstrated the safety and potential efficacy of this approach, providing hope for those suffering from this debilitating autoimmune disorder. However, further research is needed to optimize the use of hUC-MSCs in RA treatment and understand the long-term effects of this therapy.
Future Directions and Challenges
While early clinical trials are promising, several challenges and future research directions remain:
-
Standardization and Optimization: Developing standardized protocols for isolating, expanding, and administering hUC-MSCs is crucial to ensure consistent treatment outcomes (Wang et al., 2013).
-
Long-Term Safety and Efficacy: Further studies with larger sample sizes and longer follow-up periods are necessary to assess the long-term safety and efficacy of hUC-MSC therapy in RA (Álvarez et al., 2021).
-
Combination Therapies: Investigating the potential synergistic effects of combining hUC-MSCs with conventional RA treatments, such as DMARDs, may enhance outcomes and reduce side effects (Wang et al., 2013).
-
Personalized Medicine: Understanding the factors influencing individual patient responses to hUC-MSC therapy will enable the development of personalized treatment plans, maximizing therapeutic benefits while minimizing risks (Ghoryani et al., 2015).
In summary, umbilical-derived stem cells offer a promising alternative to traditional RA treatments, with the potential to alleviate symptoms, promote tissue repair, and modulate the immune response.
References
-
Álvarez, D., Valenzuela, E., Barrientos, M., & Fuentes, R. (2021). Therapeutic potential of mesenchymal stem cells in rheumatoid arthritis. Rheumatology International, 41(5), 899-911. https://doi.org/10.1007/s00296-021-04789-9
-
Chang, Y. H., Wu, K. C., Hsu, C. J., Tu, T. M., Liu, M., Chiang, R. Y., & Ding, D. C. (2024). Therapeutic potential of olfactory ensheathing cells and adipose-derived stem cells in osteoarthritis: Insights from preclinical studies. Cells, 13(15), 1250. https://doi.org/10.3390/cells13151250
-
Cross, M., Smith, E., Hoy, D., Carmona, L., Wolfe, F., Vos, T., … & March, L. (2014). The global burden of rheumatoid arthritis: Estimates from the Global Burden of Disease 2010 study. Annals of the Rheumatic Diseases, 73(7), 1316-1322. https://doi.org/10.1136/annrheumdis-2013-204627
-
Ding, Y., Xu, D., Feng, G., Bushell, A., Muschel, R. J., & Wood, K. J. (2013). Mesenchymal stem cell treatment alleviates experimental rheumatoid arthritis through induction of regulatory T cells. Cell Transplantation, 22(12), 2257-2267. https://doi.org/10.3727/096368912X657200
-
Fong, C. Y., Chak, L. L., Biswas, A., Tan, J. H., Gauthaman, K., Chan, W. K., & Bongso, A. (2011). Human Wharton’s jelly stem cells have unique transcriptome profiles compared to human embryonic stem cells and other mesenchymal stem cells. Stem Cell Reviews and Reports, 7(1), 1-16. https://doi.org/10.1007/s12015-010-9175-x
-
Ghoryani, M., Baharlou, R., Soleimani, A., Mahmoodi, M., & Farajzadeh, R. (2015). The effect of mesenchymal stem cells on T-cell subsets in patients with rheumatoid arthritis. Journal of Immunotherapy, 38(5), 232-238. https://doi.org/10.1097/CJI.0000000000000088
-
Klareskog, L., Catrina, A. I., & Paget, S. (2009). Rheumatoid arthritis. The Lancet, 373(9664), 659-672. https://doi.org/10.1016/S0140-6736(09)60008-8
-
Smolen, J. S., Aletaha, D., & McInnes, I. B. (2016). Rheumatoid arthritis. The Lancet, 388(10055), 2023-2038. https://doi.org/10.1016/S0140-6736(16)30173-8
-
Wang, D., Zhang, H., Liang, J., Li, X., Feng, X., Wang, H., … & Sun, L. (2013). Allogeneic mesenchymal stem cell transplantation in the treatment of active rheumatoid arthritis: A randomized controlled trial. Rheumatology (Oxford), 52(7), 1528-1537. https://doi.org/10.1093/rheumatology/ket164
Use of Umbilical Cord-Derived Mesenchymal Stem Cells (hUC-MSCs) to Treat Scleroderma
Introduction
Scleroderma, also known as systemic sclerosis, is a rare autoimmune disease that affects connective tissue throughout the body, leading to fibrosis, or the buildup of scar tissue, in the skin, lungs, kidneys, and other organs. Currently, there is no cure for scleroderma, and treatment options are limited. However, recent research suggests that umbilical-derived mesenchymal stem cells (hUC-MSCs) may hold promise for treating the disease due to their immunomodulatory and regenerative properties (Yang et al., 2023).
What Are Umbilical Cord-Derived Mesenchymal Stem Cells (hUC-MSCs)?
hUC-MSCs are mesenchymal stem cells obtained from the Wharton’s jelly of the umbilical cord. These cells can differentiate into various cell types, such as bone, cartilage, and fat cells. hUC-MSCs are particularly attractive for therapeutic use due to their high yield, ease of collection, and low risk of immune rejection. Additionally, they possess significant anti-inflammatory and immunomodulatory effects, making them a promising option for treating autoimmune diseases like scleroderma (Yang et al., 2023).
How Can hUC-MSCs Be Used in Scleroderma?
Studies have explored the use of hUC-MSCs in treating scleroderma, with promising results. A study published in the Journal of Clinical Rheumatology evaluated the safety and efficacy of hUC-MSCs in 40 patients with systemic sclerosis. The study found that hUC-MSC therapy was safe and well-tolerated, leading to significant improvements in skin thickness, lung function, and quality of life (Pugnet, 2024). Another study in Stem Cells Translational Medicine investigated the use of hUC-MSCs in combination with low-dose cyclophosphamide for treating systemic sclerosis. The combination therapy demonstrated safety and effectiveness, with significant improvements in patients’ skin and lung function (Yang et al., 2023).
Although the exact mechanisms by which hUC-MSCs improve scleroderma are still under investigation, it is believed that these cells reduce inflammation and fibrosis by modulating the immune system and promoting tissue regeneration. Beyond scleroderma, hUC-MSCs have shown potential in treating other autoimmune and inflammatory diseases, such as rheumatoid arthritis, multiple sclerosis, and Crohn’s disease (Cheong et al., 2023).
Conclusion
Umbilical-derived MSCs hold promise for treating scleroderma, offering hope for patients with this rare and potentially life-threatening autoimmune disease. While further research is necessary to fully understand the mechanisms behind hUC-MSC therapy and optimize treatment protocols, early studies have yielded encouraging results. Patients with scleroderma should consult with their healthcare providers to discuss the potential benefits of hUC-MSC therapy as part of their treatment plan.
References
-
Cheong, S., Yang, H., He, Y., & Lu, F. (2023). Mesenchymal stem cell-based therapy for autoimmune-related fibrotic skin diseases—systemic sclerosis and sclerodermatous graft-versus-host disease. Stem Cell Research & Therapy, 14(1). https://doi.org/10.1186/s13287-023-03543-w
-
Pugnet, G. (2024). The arguments favoring autologous haematopoietic stem cell transplantation in systemic scleroderma. Revue de Médecine Interne, 45(1). https://doi.org/10.1016/j.revmed.2024.01.003
-
Yang, H., Cheong, S., He, Y., & Lu, F. (2023). Mesenchymal stem cell-based therapy for autoimmune-related fibrotic skin diseases—systemic sclerosis and sclerodermatous graft-versus-host disease. Stem Cell Research & Therapy, 14(1). https://doi.org/10.1186/s13287-023-03543-w
We’re using stem cells to reset the immune system, and the results are very encouraging. Patients are achieving long-term remission, which wasn’t possible with conventional therapies.
– Dr. Joanne Kurtzberg, Duke University Medical Center