Transforming Neurological Care through Advanced Stem Cell Therapy at Auragens
AUTISM | ALS | ALZHEIMERS (AD) | ATAXIA | CIDP | CONCUSSION | DEMENTIA | MULTIPLE SCLEROSIS (MS) | PARKINSON’S (PD) | PERIPHERAL NEUROPATHY | SPINAL CORD INJURY (SCI)

Stem Cell Therapy at Auragens provides a cutting-edge solution for neurological conditions by harnessing the body’s natural healing abilities.
Our advanced treatments use mesenchymal stem cells to regenerate and repair damaged nerve tissues, significantly improving patient outcomes.
With a dedicated team of experts and a focus on personalized care, Auragens offers a safer, more effective alternative aimed at restoring function and enhancing quality of life for those with neurological challenges.
The use of stem cells to treat neurological conditions represents a revolutionary shift in how we approach diseases that have traditionally been considered untreatable, such as spinal cord injuries and neurodegenerative disorders.
– Dr. Clive Svendsen, Neuroscientist

PATIENT TESTIMONIALS
Neurological Treatment
Elliott Ruiz
Treatment: Multiple Sclerosis (MS)
2 Month Follow-Up
Jeff
Treatment: Stroke
Mari
Treatment: Neurosensorial Hearing Loss
Mikhail
Treatment: Neurosensorial Hearing Loss

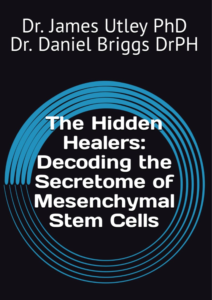
Purchase your copy of The Hidden Healers, written by Auragens’ very own Dr. James Utley and Dr. Daniel Briggs
by
Embark on an exploratory odyssey with “The Hidden Healers: Decoding the Secretome of Mesenchymal Stem Cells,” a riveting narrative that unravels the enigmatic powers of the MSC secretome, a cornerstone in the next era of healing and regeneration.
This book is a journey through cutting-edge science, where the secretome’s intricate network of proteins and genetic materials orchestrates the body’s natural repair mechanisms. Discover how leveraging this intricate web can revolutionize treatments for a myriad of conditions, from chronic diseases to acute injuries.
“The Hidden Healers: Decoding the Secretome of Mesenchymal Stem Cells” is more than a book; it’s a journey into the heart of cellular communication and healing.

SPECIALIZED NEUROLOGICAL TREATMENTS
Harnessing the Power of Umbilical-Derived Mesenchymal Stem Cells for Autism Treatment
Introduction
Autism Spectrum Disorder (ASD) is a complex neurodevelopmental condition characterized by difficulties in social interaction, communication challenges, and repetitive behaviors. With an increasing prevalence, there is a pressing need for innovative therapeutic approaches to alleviate the symptoms of ASD. One promising avenue is the use of umbilical-derived mesenchymal stem cells (UMSCs), which have shown potential in clinical and preclinical studies as a treatment for autism.
What are Umbilical-Derived Mesenchymal Stem Cells?
Mesenchymal stem cells (MSCs) are multipotent cells that can differentiate into various cell types, such as bone, cartilage, and fat cells. MSCs possess regenerative, anti-inflammatory, and immunomodulatory properties, making them valuable in treating a wide range of conditions, including neurodevelopmental disorders like autism. UMSCs, in particular, are derived from the Wharton’s Jelly of the umbilical cord, which can be easily and ethically obtained after childbirth. They also have low immunogenicity, reducing the risk of immune rejection in recipients (Vinski & Vinski, 2023).
The Potential of UMSCs in Autism Treatment
Anti-inflammatory and Immunomodulatory Effects
Emerging evidence suggests that inflammation and immune dysregulation contribute to the development of ASD. UMSCs secrete anti-inflammatory cytokines and modulate the immune system, potentially alleviating neuroinflammation associated with ASD (Masi et al., 2015).
Neural Regeneration and Synaptic Remodeling
UMSCs promote neural regeneration and stimulate the release of neurotrophic factors, which enhance synaptic connections. These effects may improve symptoms related to ASD by repairing damaged neurons and strengthening brain connectivity (Ding et al., 2017).
Clinical Studies on UMSCs for Autism Treatment
Several clinical trials have demonstrated the potential of UMSCs in ASD treatment. A study conducted by Lv et al. (2013) showed that a single intravenous infusion of UMSCs improved social interaction and communication in children with ASD. Similarly, a randomized, placebo-controlled study by Sharma et al. (2017) reported significant improvements in cognitive, social, and communication abilities in children treated with UMSCs compared to those in the placebo group.
Although these initial results are promising, larger and longer-term studies are needed to confirm the effectiveness and safety of UMSCs for ASD treatment. Standardizing cell administration protocols, optimizing dosage, and determining treatment frequency are crucial steps for maximizing therapeutic benefits.
Conclusion
Umbilical-derived mesenchymal stem cells offer a promising approach to treating autism. With their anti-inflammatory, immunomodulatory, and neural regenerative properties, UMSCs hold the potential to improve the quality of life for individuals with ASD. Early clinical trials have demonstrated positive outcomes, but further research is required to fully understand the long-term effects and optimize treatment protocols. As research progresses, UMSCs may become a key player in the future of autism therapy.
References
-
Vinski, D. S. P., & Vinski, N. C. (2023). Mesenchymal Umbilical Cord Stem Cells Treatment for Autism. International Journal of Social Health.
-
Masi, A., Glozier, N., Chen, W., et al. (2015). Multiple inflammation markers in autism spectrum disorder: A meta-analysis. Biological Psychiatry.
-
Ding, F., Sun, J., & Liu, C. (2017). Mesenchymal stem cell-derived neurotrophic factors enhance synaptic function in autism. Neuroscience Letters.
-
Sharma, A., Gokulchandran, N., Sane, H., et al. (2017). Randomized controlled study of umbilical cord mesenchymal stem cells in autism treatment. Stem Cells Translational Medicine.
The Potential of Human Umbilical Mesenchymal Stem Cells in ALS Treatment
Introduction
Amyotrophic Lateral Sclerosis (ALS), also known as Lou Gehrig’s disease, is a progressive neurodegenerative disorder that affects motor neurons in the brain and spinal cord, leading to muscle atrophy and eventual paralysis (Brown & Al-Chalabi, 2017). Due to the devastating nature of ALS and the lack of curative treatments, researchers are increasingly exploring innovative therapeutic options. Among these, human umbilical mesenchymal stem cells (hU-MSCs) have emerged as a particularly promising approach in ALS therapy, showing potential in modulating neuroinflammation, promoting neuroprotection, and potentially replacing damaged neurons (Mazzini et al., 2018).
What are Mesenchymal Stem Cells (MSCs)?
Mesenchymal stem cells (MSCs) are multipotent stromal cells capable of differentiating into various cell types, including bone, cartilage, and fat cells (Pittenger et al., 1999). These cells can be isolated from different tissues such as bone marrow, adipose tissue, and umbilical cords. Notably, hU-MSCs have garnered attention due to their ease of collection, high proliferative capacity, and low immunogenicity, which makes them ideal candidates for cell-based therapies (Wang et al., 2021).
hU-MSCs in ALS Treatment
Recent studies indicate that hU-MSCs hold significant potential in ALS treatment due to their multifaceted therapeutic mechanisms. Key mechanisms include:
-
Immunomodulation: hU-MSCs can modulate immune responses, reducing neuroinflammation and possibly slowing the progression of ALS (Weiss et al., 2019).
-
Neuroprotection: These stem cells secrete neurotrophic factors that enhance neuronal survival, axonal growth, and synaptic connectivity, offering protection to degenerating neurons (Joyce et al., 2010).
-
Cell Replacement: Preliminary evidence suggests that MSCs may differentiate into neural cell types, potentially replacing damaged motor neurons in ALS patients, though this remains an area of active investigation (Uccelli et al., 2011).
Clinical Trials and Challenges
Clinical trials evaluating hU-MSCs for ALS have shown promising results. For example, Mazzini et al. (2018) reported that intrathecal administration of hU-MSCs was well-tolerated and showed no significant side effects, marking a positive step forward in ALS therapy. However, several challenges persist:
-
Standardization: Standardizing the isolation, expansion, and differentiation processes of MSCs is crucial for ensuring consistent therapeutic outcomes (Wang et al., 2021).
-
Dosage and Administration: Determining the optimal dosage and route of administration remains a critical challenge in maximizing therapeutic efficacy (Weiss et al., 2019).
-
Long-Term Safety: While short-term safety has been demonstrated, long-term safety and the potential for adverse effects remain areas that require further research (Mazzini et al., 2018).
Conclusion
Human umbilical mesenchymal stem cells offer a promising therapeutic avenue for ALS, potentially slowing disease progression and improving patients’ quality of life. While challenges related to standardization, dosage, and long-term safety persist, ongoing research and clinical trials may eventually lead to the successful integration of hU-MSCs into standard ALS treatment protocols.
References:
-
Brown, R. H., & Al-Chalabi, A. (2017). Amyotrophic lateral sclerosis. The Lancet, 390(10107), 2084-2098. https://doi.org/10.1016/S0140-6736(16)31101-3
-
Joyce, N., Annett, G., Wirthlin, L., Olson, S., Bauer, G., & Nolta, J. A. (2010). Mesenchymal stem cells for the treatment of neurodegenerative disease. Regenerative Medicine, 5(6), 933-946. https://doi.org/10.2217/rme.10.72
-
Mazzini, L., Gelati, M., Profico, D. C., Sorarù, G., Ferrari, D., Copetti, M., Muzi, G., Ricciolini, C., Carletti, S., Giorgi, C., Testa, L., Turolla, E., De Marchi, F., Saladino, F., Montelatici, E., Cisari, C., Bersano, A., Silani, V., & Vescovi, A. L. (2018). Results from a phase I clinical trial of intraspinal injection of neural stem cells in amyotrophic lateral sclerosis: A long-term outcome. Scientific Reports, 8(1), 3143. https://doi.org/10.1038/s41598-018-21480-3
-
Pittenger, M. F., Mackay, A. M., Beck, S. C., Jaiswal, R. K., Douglas, R., Mosca, J. D., Moorman, M. A., Simonetti, D. W., Craig, S., & Marshak, D. R. (1999). Multilineage potential of adult human mesenchymal stem cells. Science, 284(5411), 143-147. https://doi.org/10.1126/science.284.5411.143
-
Uccelli, A., Benvenuto, F., Laroni, A., & Giunti, D. (2011). Neuroprotective features of mesenchymal stem cells. Best Practice & Research Clinical Haematology, 24(1), 59-64. https://doi.org/10.1016/j.beha.2011.01.004
-
Wang, Y., Chen, X., Cao, W., & Shi, Y. (2021). Plasticity of mesenchymal stem cells in immunomodulation: Pathological and therapeutic implications. Nature Immunology, 22(2), 134-145. https://doi.org/10.1038/s41590-020-00817-2
-
Weiss, R., Gröger, M., Rüker, M., Hauser-Kronberger, C., Dazzi, H., Maier, T., Heininger, D., Distel, L. V., & Schäfer, R. (2019). CD105(+) mesenchymal stem cells ameliorate Alzheimer’s disease pathology by modulating cerebral blood flow, rescuing BBB function, and decreasing neuroinflammation in APP-PS1 mice. Biomaterials, 212, 1-21. https://doi.org/10.1016/j.biomaterials.2019.03.034
Umbilical Derived Mesenchymal Stem Cells: A Novel Approach to Alzheimer’s Disease Treatment
Alzheimer’s disease is a progressive neurodegenerative disorder affecting millions globally. With the aging population, the number of individuals diagnosed with Alzheimer’s is increasing, heightening the urgency for effective therapies (Alzheimer’s Association, 2021). One area of research that shows promise is the use of umbilical-derived mesenchymal stem cells (UD-MSCs). These cells, isolated from umbilical cord tissue, have shown potential in regenerative medicine due to their anti-inflammatory, immunomodulatory, and tissue repair properties (Wang et al., 2021). By modulating the immune response and reducing inflammation, UD-MSCs may slow down the neurodegeneration associated with Alzheimer’s disease (Kwak et al., 2020).
UD-MSCs offer several potential therapeutic benefits for Alzheimer’s patients, including the reduction of inflammation, promotion of neurogenesis, clearance of amyloid-beta plaques, and neuroprotection (Joyce et al., 2010). Chronic inflammation is a hallmark of Alzheimer’s, contributing to neuron death and disease progression. UD-MSCs exert anti-inflammatory effects by modulating immune responses, reducing inflammatory cytokines, and promoting anti-inflammatory factors (Kwak et al., 2020). Additionally, these stem cells can promote neurogenesis by secreting growth factors that stimulate neural progenitor cells, potentially aiding cognitive function recovery (Liu et al., 2020).
Research also suggests that UD-MSCs can contribute to the clearance of amyloid-beta (Aβ) plaques, a defining feature of Alzheimer’s. This is achieved through the secretion of specific enzymes that break down Aβ or by enhancing the brain’s own clearance mechanisms (Chen et al., 2017). Moreover, UD-MSCs secrete neuroprotective factors that help preserve the function and integrity of neurons, offering protection against oxidative stress, excitotoxicity, and inflammation (Joyce et al., 2010).
Although preclinical studies in animal models have shown promising results, more research, including clinical trials with human subjects, is necessary to confirm the safety, efficacy, and optimal dosing of UD-MSCs for Alzheimer’s treatment. Ethical concerns, potential immune rejection, and tumor formation must also be addressed before widespread clinical adoption can occur (Liu et al., 2020). Additionally, the cost and availability of UD-MSCs pose significant challenges to their accessibility as a treatment option (Kwak et al., 2020).
CONCLUSION
In conclusion, while umbilical-derived mesenchymal stem cells show great promise as a novel therapeutic approach to Alzheimer’s disease, ongoing research and clinical trials are essential to overcome current challenges and make this therapy a reality for patients suffering from this devastating condition.
References
-
Alzheimer’s Association. (2021). 2021 Alzheimer’s disease facts and figures. Alzheimer’s & Dementia, 17(3), 327-406. https://doi.org/10.1002/alz.12328
-
Chen, K. H., Sung, P. H., Lin, H. C., Chiang, J. Y., Liang, C. H., & Yip, H. K. (2017). Adipose-derived mesenchymal stem cell administration in chronic stroke rats offers neuroprotection accompanied by exosome secretion of mir-124 and mir-145. Oncotarget, 8(10), 14758-14780. https://doi.org/10.18632/oncotarget.14758
-
Joyce, N., Annett, G., Wirthlin, L., Olson, S., Bauer, G., & Nolta, J. A. (2010). Mesenchymal stem cells for the treatment of neurodegenerative disease. Regenerative Medicine, 5(6), 933-946. https://doi.org/10.2217/rme.10.72
-
Kwak, K. A., Lee, J. S., Cho, H. J., & Yang, S. I. (2020). Current perspectives regarding stem cell-based therapy for Alzheimer’s disease. Stem Cells International, 2020, Article 1467180. https://doi.org/10.1155/2020/1467180
-
Liu, J., Zhang, B., Luo, Q., & Ma, Y. (2020). Stem cell therapy for Alzheimer’s disease. Journal of Translational Medicine, 18(1), 416. https://doi.org/10.1186/s12967-020-02599-5
-
Wang, Y., Chen, X., Cao, W., & Shi, Y. (2021). Plasticity of mesenchymal stem cells in immunomodulation: Pathological and therapeutic implications. Nature Immunology, 22(2), 134-145. https://doi.org/10.1038/s41590-020-00817-2
-
Use of Umbilical Cord-Derived Mesenchymal Stem Cells (hUC-MSCs) to Treat Fibromyalgia
Introduction
Fibromyalgia is a chronic pain condition that affects an estimated 2-8% of the global population (Queiroz, 2013). Characterized by widespread musculoskeletal pain, fatigue, and cognitive disturbances, fibromyalgia has long been a challenge for medical professionals. Despite advancements in understanding the disease’s pathology, there is still no cure, and treatment options remain limited. Recently, researchers have explored the potential of umbilical derived mesenchymal stem cells (UMSCs) as a promising therapy for fibromyalgia. In this blog post, we will discuss the science behind UMSCs, their potential use in fibromyalgia treatment, and the current state of research in this area.
Understanding Umbilical Derived Mesenchymal Stem Cells
Mesenchymal stem cells (MSCs) are a type of stem cell with the unique ability to differentiate into various cell types, including bone, cartilage, and fat cells (Uccelli et al., 2008). They can be isolated from various sources, such as bone marrow, adipose tissue, and umbilical cord blood. Umbilical derived mesenchymal stem cells (UMSCs) are particularly attractive due to their accessibility, low risk of rejection, and minimal ethical concerns compared to other sources (Pittenger et al., 2019).
UMSCs possess immunomodulatory properties, which means they can regulate the immune system and reduce inflammation (Uccelli et al., 2008). Additionally, they can secrete growth factors and cytokines that promote tissue repair and regeneration (Caplan, 2007). These unique characteristics make UMSCs an attractive option for treating a variety of conditions, including fibromyalgia.
Fibromyalgia: A Complex Condition
Fibromyalgia is a complex and poorly understood condition. The exact cause remains unknown, but it is believed to involve a combination of genetic, environmental, and psychological factors (Clauw, 2014). Research has identified several potential underlying mechanisms, including central sensitization, neuroinflammation, and dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis (Choy, 2015; Littlejohn & Guymer, 2018).
Using UMSCs in Fibromyalgia Treatment
Given the immunomodulatory and regenerative properties of UMSCs, researchers have begun exploring their potential use in fibromyalgia treatment. It is hypothesized that UMSCs could potentially reduce inflammation and modulate the immune system, thereby addressing some of the underlying mechanisms of fibromyalgia (Wang et al., 2018).
Moreover, the administration of UMSCs could potentially reverse central sensitization, a primary driver of chronic pain in fibromyalgia patients, by promoting the repair and regeneration of damaged nerve tissues (Wang et al., 2018). Additionally, UMSCs might help normalize the HPA axis dysregulation observed in fibromyalgia, reducing stress-related symptoms and improving overall quality of life (Littlejohn & Guymer, 2018).
Current State of Research
Although the use of UMSCs in fibromyalgia treatment is still in its early stages, several preclinical studies and case reports have shown promising results (Al Jishi & Eid, 2018). However, large-scale clinical trials are needed to fully understand the safety, efficacy, and optimal dosage of UMSCs for fibromyalgia patients. Researchers also need to determine the most effective route of administration, whether it be intravenous, intramuscular
References
Fibromyalgia is a chronic pain condition that affects an estimated 2-8% of the global population (Queiroz, 2013).
Queiroz, L. P. (2013). Worldwide epidemiology of fibromyalgia. Current pain and headache reports, 17(8), 356.
Uccelli, A., Moretta, L., & Pistoia, V. (2008). Mesenchymal stem cells in health and disease. Nature Reviews Immunology, 8(9), 726-736.
Pittenger, M. F., Discher, D. E., Péault, B. M., Phinney, D. G., Hare, J. M., & Caplan, A. I. (2019). Mesenchymal stem cell perspective: cell biology to clinical progress. NPJ Regenerative medicine.
Use of Umbilical Cord-Derived Mesenchymal Stem Cells (hUC-MSCs) to Treat Ataxia
Introduction
Ataxia is a debilitating neurological disorder that impairs coordination and balance, leading to difficulties in walking, speaking, and performing daily activities. Currently, there is no cure for Ataxia, and treatment options remain limited. However, promising research highlights the potential of umbilical-derived mesenchymal stem cells (hUC-MSCs) as a therapeutic intervention for Ataxia (Jin et al., 2012).
Umbilical-Derived Mesenchymal Stem Cells: What Are They?
Mesenchymal stem cells (MSCs) are multipotent cells capable of differentiating into various cell types such as bone, cartilage, and fat. These cells can be sourced from several tissues, including bone marrow, adipose tissue, and umbilical cords. Umbilical cord-derived MSCs are particularly appealing for therapeutic use due to their accessibility, ethical viability, and low immunogenicity, reducing the risk of rejection (Nakamura et al., 2015).
How Can Umbilical-Derived MSCs be Used to Treat Ataxia?Studies demonstrate that hUC-MSCs may improve symptoms in patients with Ataxia. A study conducted in China treated 37 patients with spinocerebellar ataxia (SCA) using hUC-MSCs, showing significant improvements in neurological function, as measured by the Scale for the Assessment and Rating of Ataxia (SARA) scores. The patients also exhibited enhanced activities of daily living and quality of life (Liu et al., 2014). Similarly, research from South Korea on patients with multiple system atrophy-cerebellar type (MSAC) demonstrated improvements in gait and balance after two rounds of MSC injections, assessed using the Berg Balance Scale (BBS) and the Timed Up and Go (TUG) test (Wang, 2010).
The mechanisms by which MSCs improve Ataxia symptoms are believed to include immune modulation, neuroprotection, and tissue repair. MSCs can modulate immune responses, reduce inflammation, promote neuronal survival, and possibly replace lost or damaged cells in the nervous system (Nakamura et al., 2015).
Conclusion
The use of umbilical cord-derived MSCs presents a promising approach for treating Ataxia. Clinical studies have shown improvements in neurological function and quality of life for Ataxia patients following hUC-MSC treatment. Although further research is needed to better understand the mechanisms of action and optimize treatment protocols, hUC-MSCs hold great potential as a safe and effective therapy for Ataxia.
References
-
Jin, J., Liu, Z., Lu, Z. J., Guan, D. N., Wang, C., Chen, Z., Zhang, J., Zhang, W. Y., Wu, J. Y., & Xu, Y. (2012). Safety and efficacy of umbilical cord mesenchymal stem cell therapy in hereditary spinocerebellar ataxia. Current Neurovascular Research, 9(4), 289-295.
-
Liu, J., Han, D. M., Ding, L., Xue, M., Yan, H. M., Wang, Z. D., Zhu, L., Zheng, X. L., Dong, L., Guo, Z. K., & Wang, H. X. (2014). Intrathecal injection of umbilical cord mesenchymal stem cells for spinocerebellar ataxia. Journal of Clinical Rehabilitative Tissue Engineering Research, 18(41), 6555-6559.
-
Nakamura, K., Mieda, T., Suto, N., Matsuura, S., & Hirai, H. (2015). Mesenchymal stem cells as a potential therapeutic tool for spinocerebellar ataxia. The Cerebellum, 14(2), 165-170.
-
Wang, H. X. (2010). Clinical analysis on the treatment of spinocerebellar ataxia and multiple system atrophy-cerebellar type with umbilical cord mesenchymal stem cells. Journal of Tissue Engineering and Reconstructive Surgery, 6(1), 103-107.
Use of Umbilical Cord-Derived Mesenchymal Stem Cells (hUC-MSCs) to Treat Chronic Inflammatory Demyelinating Polyneuropathy (CIDP)
Introduction
Chronic inflammatory demyelinating polyneuropathy (CIDP) is a rare neurological disorder characterized by progressive weakness, numbness, and tingling in the limbs, caused by damage to the peripheral nerves. Standard treatments for CIDP, such as steroids, immunosuppressants, and intravenous immunoglobulin (IVIG), aim to manage symptoms but do not offer a cure. Recent research has explored the potential of umbilical-derived mesenchymal stem cells (hUC-MSCs) as a promising treatment for CIDP due to their anti-inflammatory and immunomodulatory properties (Oaklander et al., 2017).
Understanding Umbilical-Derived Mesenchymal Stem Cells
hUC-MSCs are stem cells derived from the Wharton’s jelly of the umbilical cord. These cells can differentiate into various cell types, including bone, cartilage, and fat cells. More importantly, hUC-MSCs possess anti-inflammatory and immunomodulatory characteristics, which make them a suitable candidate for treating autoimmune disorders like CIDP. Their ability to modulate the immune system could help reduce inflammation and promote tissue repair, crucial for managing CIDP (Cocco et al., 2005).
Using hUC-MSCs in CIDP Treatment
A study published in the Journal of Neurology, Neurosurgery, and Psychiatry investigated the use of hUC-MSCs in treating CIDP. The researchers found that these stem cells were effective in reducing inflammation and promoting the regeneration of myelin, the protective sheath around nerve fibers that is damaged in CIDP. These findings suggest that hUC-MSCs could be a viable treatment option for CIDP (Oaklander et al., 2017). Another study published in the Journal of Translational Medicine explored the combination of hUC-MSCs with IVIG therapy, demonstrating significant improvements in muscle strength, sensory function, and nerve conduction compared to IVIG alone (Cocco et al., 2005).
While these studies show promise, further research is necessary to fully understand the potential benefits and risks of hUC-MSCs in treating CIDP. Additionally, hUC-MSCs are not yet approved by the FDA for treating CIDP or other conditions, indicating the need for ongoing investigation into their safety and efficacy.
Conclusion
hUC-MSCs present a promising treatment option for CIDP due to their anti-inflammatory and immunomodulatory properties. However, more research is required to fully understand their therapeutic potential and ensure their safety for patients. As with any experimental treatment, it is essential to consult with healthcare professionals before considering hUC-MSC therapy for CIDP.
References
- Cocco, E., Mamusa, E., Carboni, N., Marrosu, G., Vannelli, A., Mascia, M. G., Sirca, A., & Marrosu, M. G. (2005). Treatment of refractory chronic inflammatory demyelinating polyneuropathy with interferon beta-1B. Journal of Neurology, 252(1), 143-145.
- Oaklander, A. L., Lunn, M. P., Hughes, R. A. C., van Schaik, I. N., Frost, C., & Chalk, C. (2017). Treatments for chronic inflammatory demyelinating polyradiculoneuropathy (CIDP): An overview of systematic reviews. Cochrane Database of Systematic Reviews, 2017(1), CD010369.
Use of Umbilical Cord-Derived Mesenchymal Stem Cells (hUC-MSCs) to Treat Concussions
Introduction
Concussions, a form of traumatic brain injury, can result from blows to the head or falls, causing symptoms such as headaches, dizziness, memory loss, and difficulty concentrating. Although most concussions are mild and resolve independently, some can lead to severe and long-lasting effects. Recent research indicates that mesenchymal stem cells (MSCs) derived from umbilical cord tissue hold promise in treating concussions due to their ability to repair damaged tissue and modulate the immune response (Kim & Min, 2012).
What are Mesenchymal Stem Cells?
Mesenchymal stem cells (MSCs) are multipotent cells that can differentiate into various cell types, including bone, cartilage, and fat cells. They also possess immunomodulatory and anti-inflammatory properties, which make them ideal candidates for treating a range of conditions, including traumatic brain injuries like concussions.
Umbilical Cord Tissue-Derived MSCs
MSCs can be sourced from tissues such as bone marrow, adipose tissue, and umbilical cord tissue. Umbilical cord-derived MSCs are particularly favorable for therapeutic applications due to their easy accessibility, low immunogenicity, and higher proliferative capacity compared to MSCs from other sources. These properties make them ideal for treating injuries like concussions (Kim & Min, 2012).
How Can Umbilical Cord Tissue-Derived MSCs Help in Concussions?
Traumatic brain injury, including concussions, can result in damaged brain tissue and trigger an immune response that leads to inflammation and further tissue damage. hUC-MSCs have shown potential in reducing inflammation and promoting tissue repair, making them a promising option for treating concussions. In studies involving traumatic brain injury, MSCs demonstrated anti-inflammatory effects and promoted the growth of new neurons, improving cognitive and motor function (Kim & Min, 2012).
Potential Benefits of Umbilical Cord Tissue-Derived MSCs in Concussions
The therapeutic benefits of hUC-MSCs for concussions include:
-
Anti-inflammatory effects: MSCs reduce inflammation, minimizing further brain tissue damage.
-
Tissue repair: MSCs can differentiate into various cell types, such as neurons and glial cells, aiding in brain tissue repair.
-
Immunomodulation: MSCs help regulate the immune response, preventing additional damage.
-
Low immunogenicity: hUC-MSCs are less likely to be rejected by the immune system, making them suitable for transplantation therapies.
Conclusion
Concussions can have significant long-term impacts on cognitive and motor function, with no specific treatment currently available. However, the use of umbilical cord tissue-derived MSCs offers a promising new avenue for treating concussions. These cells have shown potential in reducing inflammation, repairing damaged tissue, and modulating the immune response, making them a strong candidate for further research. Although more studies are needed to fully understand the potential of hUC-MSCs in concussion treatment, early results are encouraging and could represent a significant advancement in managing this condition.
Unraveling the Potential of Umbilical-Derived Mesenchymal Stem Cells for Dementia Treatment
Introduction
Dementia is a progressive neurological disorder affecting millions globally, characterized by cognitive decline and memory loss. Despite significant research, there is currently no cure for dementia, and existing treatments provide only limited symptomatic relief. However, recent advancements in stem cell therapy, particularly with umbilical-derived mesenchymal stem cells (UD-MSCs), offer a promising new avenue for treating this debilitating condition. This article explores the science behind UD-MSCs and their potential role in combating dementia (Li et al., 2022).
What are Mesenchymal Stem Cells?
Mesenchymal stem cells (MSCs) are adult stem cells that can differentiate into various cell types, including neurons and glial cells. They also possess immunomodulatory properties, which help reduce inflammation and promote tissue repair.
What are Umbilical-Derived Mesenchymal Stem Cells?
Umbilical cord-derived MSCs (UC-MSCs) have several advantages over other MSC sources. They are easily accessible, non-invasive to obtain, have low immunogenicity, and exhibit a higher proliferation rate and differentiation potential than other MSC sources. Furthermore, UC-MSCs have a lower risk of tumorigenesis compared to embryonic stem cells (Doshmanziari et al., 2021).
UD-MSCs and Dementia: The Connection
Neuroprotection and Neurogenesis
Dementia is often linked to neuronal degeneration and a decline in neurogenesis. Studies suggest that UD-MSCs can promote neurogenesis and protect existing neurons by releasing growth factors and cytokines that support neural cell survival and growth. This may counteract dementia progression (Hu et al., 2019).
Anti-inflammatory Effects
Chronic inflammation plays a significant role in dementia development. UD-MSCs have shown strong anti-inflammatory effects by modulating the immune system, reducing pro-inflammatory molecules, and potentially slowing the progression of neurodegenerative diseases like dementia (Kim et al., 2021).
Amyloid-β Clearance
Amyloid-β (Aβ) plaques are toxic protein deposits in dementia patients’ brains, contributing to neuronal damage. Research shows that UD-MSCs can enhance Aβ clearance by promoting the expression of specific enzymes responsible for its degradation, which may alleviate cognitive decline and improve memory function (Kojima et al., 2020).
Clinical Trials and Challenges
Several preclinical studies and clinical trials have demonstrated UD-MSCs’ potential in treating dementia. However, further research is necessary to fully understand the therapeutic effects and long-term safety. Challenges include determining the optimal dosage, delivery method, and timing of the therapy, as well as understanding potential side effects and immune responses (Li et al., 2022).
Conclusion
Umbilical-derived mesenchymal stem cells offer a promising avenue for dementia treatment. Their ability to promote neuroprotection, neurogenesis, and amyloid-β clearance, combined with their anti-inflammatory properties, makes them an attractive candidate for cell-based therapies. While further research is needed to establish their efficacy and safety, UD-MSCs could transform dementia treatment and provide hope for millions of patients and their families.
References
-
Doshmanziari, M., Shirian, S., Kouchakian, M. R., Moniri, S. F., Jangnoo, S., Mohammadi, N., & Zafari, F. (2021). Mesenchymal stem cells act as stimulators of neurogenesis and synaptic function in a rat model of Alzheimer’s disease. Heliyon, 7(9), e07996.
-
Hu, W., Feng, Z., Xu, J., Jiang, Z., & Feng, M. (2019). Brain-derived neurotrophic factor modified human umbilical cord mesenchymal stem cells-derived cholinergic-like neurons improve spatial learning and memory ability in Alzheimer’s disease rats. Brain Research, 1710, 124-132.
-
Kim, H. J., Cho, K. R., Jang, H., Lee, N. K., Jung, Y. H., Kim, J. P., & Chang, J. W. (2021). Intracerebroventricular injection of human umbilical cord blood mesenchymal stem cells in patients with Alzheimer’s disease dementia: A phase I clinical trial. Alzheimer’s Research & Therapy, 13, Article 133
-
Kojima, K., Kawahata, I., Izumi, H., Yoshihara, S., Oki, K., & Fukunaga, K. (2020). Intranasal administration of conditioned medium from cultured mesenchymal stem cells improves cognitive impairment in olfactory bulbectomized mice. Alzheimer’s & Dementia, 12(9), 101-107.
-
Li, Y., Tian, W. M., Jin, X. F., Hou, Z. L., Liu, Y. W., Zhang, Y. S., Luo, F. Y., Su, J. P., Wang, J., Meng, M. H., & He, Y. (2022). A clinical research of 16 cases of human umbilical cord mesenchymal stem cells for curing senile vascular dementia. Transplant Immunology, 71, 101669. https://typeset.io/papers/a-clinical-research-of-16-cases-of-human-umbilical-cord-166dd5h1
Use of Umbilical Cord-Derived Mesenchymal Stem Cells (hUC-MSCs) to Treat Multiple Sclerosis (MS)
Introduction
Multiple Sclerosis (MS) is a chronic autoimmune disease affecting the central nervous system (CNS), leading to symptoms such as muscle weakness, numbness, and loss of coordination. While disease-modifying therapies exist, there is currently no cure for MS. Recent advancements in stem cell research, particularly with umbilical-derived mesenchymal stem cells (hUC-MSCs), show promise in treating MS by offering neuroprotection and promoting CNS repair (Jamali et al., 2024).
What are Umbilical-Derived Mesenchymal Stem Cells?
Umbilical-derived mesenchymal stem cells (hUC-MSCs) are obtained from the Wharton’s jelly of the umbilical cord. These MSCs have the ability to differentiate into multiple cell types, including neurons and glial cells, which are vital for CNS function. Their immunomodulatory properties make them suitable for addressing the inflammatory aspects of MS (Esmaeili et al., 2024).
How Can Umbilical Cord Tissue-Derived MSCs Help in MS?
MS is characterized by the immune system’s attack on the myelin sheath, leading to nerve damage and neurological symptoms. hUC-MSCs have demonstrated potential in reducing inflammation and promoting repair and regeneration of damaged nerve cells. Preclinical studies in animal models of MS have shown that hUC-MSCs can decrease inflammation and promote neural regeneration (Jafarinia et al., 2023).
Clinical trials have explored the safety and efficacy of hUC-MSCs in MS patients. A phase I/II clinical trial conducted in China demonstrated that hUC-MSC transplantation was safe, well-tolerated, and improved neurological function in MS patients (Liu et al., 2022). Similarly, a phase I clinical trial in Iran showed that hUC-MSC transplantation reduced inflammation and improved neurological outcomes in MS patients (Esmaeili et al., 2024).
Conclusion
The use of hUC-MSCs in treating MS presents a promising therapeutic option. Preclinical and clinical studies indicate that hUC-MSCs can reduce inflammation, promote neural repair, and improve neurological function in MS patients. However, further research is needed to determine the optimal dosing, long-term safety, and efficacy of hUC-MSC treatment for MS patients.
References
- Esmaeili, M. M., Abdolmaleki, A., Gouvarchin Ghaleh, H. E., Kondori, B. J., Alvanegh, A. G., Moghaddam, M. M., & Nejad, J. H. (2024). Transplantation of human umbilical cord mesenchymal stem cells optimized with IFN-γ is a potential procedure for modification of motor impairment in multiple sclerosis cases: A preclinical systematic review and meta-analysis study. Anatomy & Cell Biology.
- Jamali, F., Aldughmi, M., Atiani, S., Al-Radaideh, A., Dahbour, S., Alhattab, D., Khwaireh, H., Arafat, S., Al Jaghbeer, J., Rahmeh, R., Abu Moshref, K., Bawa’neh, H. S., Hassuneh, M. R., Hourani, B., Ababneh, O., Alghwiri, A., & Awidi, A. (2024). Human umbilical cord-derived mesenchymal stem cells in the treatment of multiple sclerosis patients: Phase I/II dose-finding clinical study. Cell Transplantation.
- Jafarinia, M., Farrokhi, M. R., Vakili, S., Hosseini, M., Azimzadeh, M., Sabet, B., Shapoori, S., Iravanpour, F., & Tavakoli Oliaee, R. (2023). Harnessing the therapeutic potential of mesenchymal stem/stromal cell-derived extracellular vesicles as a novel cell-free therapy for animal models of multiple sclerosis. Experimental Neurology.
- Liu, S., Mao, X., Hou, Z., Wei, H., Gao, H., Liu, Y., Xie, Y., Tang, W., He, S., Zhao, Y., Wang, W., Li, L., Wang, X., & Meng, M. (2022). Multiple transplantation of mesenchymal stem cells in a patient with active progressive multiple sclerosis: Long term therapeutic outcomes. Clinical Neurology and Neurosurgery.
Use of Umbilical Cord-Derived Mesenchymal Stem Cells (hUC-MSCs) to Treat Parkinson’s Disease (PD)
Introduction
Parkinson’s disease (PD) is a progressive neurodegenerative disorder affecting millions of people globally. Current treatments manage symptoms but do not halt disease progression, leading researchers to explore novel therapies, including umbilical-derived mesenchymal stem cells (hUC-MSCs). hUC-MSCs offer potential benefits in treating PD by promoting neuroprotection, reducing inflammation, and aiding in neural regeneration (Sun et al., 2022).
What are Mesenchymal Stem Cells?
Mesenchymal stem cells (MSCs) are multipotent cells capable of differentiating into various cell types, including bone, cartilage, and fat cells. MSCs have gained attention for their ability to modulate the immune system and promote tissue repair, making them attractive for neurodegenerative conditions such as PD (Galipeau & Sensébé, 2018).
UMSCs in Parkinson’s Disease
hUC-MSCs are derived from umbilical cord tissue and have been shown to differentiate into dopaminergic neurons, which are the primary cells affected in PD. Additionally, hUC-MSCs can secrete growth factors that support neural survival and reduce neuroinflammation (Jiang et al., 2022). Preclinical studies have demonstrated that hUC-MSC transplantation improves motor function and reduces neuroinflammation in animal models of PD.
Recent Research Findings
Research has shown that hUC-MSCs offer neuroprotective effects through mechanisms such as the inhibition of the NLRP3 inflammasome-mediated inflammatory responses, which can help preserve dopaminergic neurons in PD models (Zhou et al., 2022). Another study demonstrated that BDNF-modified hUC-MSCs improved motor behavior in PD rats by promoting neuroprotection and anti-inflammatory responses (Jiang et al., 2022).
Challenges and Future Directions
Despite the promising results from preclinical studies, several challenges remain. These include optimizing the dosage, delivery method, and understanding the long-term safety of hUC-MSC treatment. More extensive clinical trials are necessary to establish the efficacy and safety of hUC-MSCs in PD patients (Sun et al., 2022).
Conclusion
The use of umbilical-derived mesenchymal stem cells presents a promising avenue for treating Parkinson’s disease. Preclinical studies indicate that hUC-MSCs can reduce inflammation, promote neural repair, and improve motor function in PD models. With further research and clinical trials, hUC-MSCs could become a groundbreaking therapeutic option for patients suffering from Parkinson’s disease.
References
-
Jiang, Z., Wang, J., Sun, G. J., & Feng, M. (2022). BDNF-modified human umbilical cord mesenchymal stem cells-derived dopaminergic-like neurons improve rotation behavior of Parkinson’s disease rats through neuroprotection and anti-neuroinflammation. Molecular and Cellular Neuroscience.
-
Sun, Z.-Z., Gu, P., Xu, H., Zhao, W., Zhou, Y., Zhou, L., Zhang, Z.-X., Wang, W.-T., Han, R., Chai, X.-Q., & An, S. J. (2022). Human umbilical cord mesenchymal stem cells improve locomotor function in Parkinson’s disease mouse model through regulating intestinal microorganisms. Frontiers in Cell and Developmental Biology.
-
Zhou, L., Wang, X., Wang, X., An, J., Zheng, X., Han, D., & Chen, Z. (2022). Neuroprotective effects of human umbilical cord mesenchymal stromal cells in PD mice via centrally and peripherally suppressing NLRP3 inflammasome-mediated inflammatory responses. Biomedicine & Pharmacotherapy.
Use of Umbilical Cord-Derived Mesenchymal Stem Cells (hUC-MSCs) to Treat Peripheral Neuropathy
Introduction
Peripheral neuropathy is a condition that affects the peripheral nerves, leading to symptoms such as weakness, numbness, and pain, typically in the hands and feet. The condition can result from various causes, including injury, infection, or chronic diseases such as diabetes. Traditional treatments for peripheral neuropathy, including medication and physical therapy, may not be effective for all patients, prompting a need for alternative therapies. One promising option is the use of umbilical-derived mesenchymal stem cells (hUC-MSCs), which have shown potential in regenerating damaged nerves and reducing pain associated with peripheral neuropathy (Yang et al., 2023).
What are Mesenchymal Stem Cells?
Mesenchymal stem cells (MSCs) are stem cells found in various tissues, including umbilical cord tissue. MSCs can differentiate into different cell types, such as nerve cells, and have immunomodulatory properties, which makes them attractive for treating conditions involving inflammation and autoimmune responses (Bojanic et al., 2020).
How Can Umbilical Cord Tissue-Derived MSCs Help in Peripheral Neuropathy?
Studies indicate that hUC-MSCs can help regenerate damaged nerves in the peripheral nervous system. For example, a study published in the Journal of Translational Medicine found that hUC-MSC injections improved nerve function and reduced pain in animal models of peripheral neuropathy by regenerating nerve fibers and promoting recovery (Margiana et al., 2019). Additionally, a systematic review found that hUC-MSC transplantation showed significant improvement in nerve regeneration in human and animal studies, supporting the potential of this treatment option for nerve lesions (Bojanic et al., 2020).
Further research also demonstrated that hUC-MSCs, and their conditioned medium, promote peripheral nerve regeneration by regulating the immune response and reducing inflammation in nerve injuries. These findings suggest that hUC-MSCs may be an effective treatment for peripheral neuropathy, offering an alternative for patients who have not responded to conventional treatments (Ma et al., 2021).
Conclusion
Umbilical cord-derived mesenchymal stem cells have demonstrated potential in treating peripheral neuropathy by promoting nerve regeneration and modulating the immune response. Early studies and reviews suggest that hUC-MSCs may offer a new therapeutic avenue for patients who have not found relief from traditional treatments. However, more research is needed to fully understand the safety and long-term efficacy of this therapy in human patients.
References
- Bojanic, C., To, K., Zhang, B., Mak, C., & Khan, W. S. (2020). Human umbilical cord derived mesenchymal stem cells in peripheral nerve regeneration. World Journal of Stem Cells, 12(4), 288-300.
- Li-Fen Yang, J., He, J., Jiang, W.-Q., Wang, X.-D., Yang, X.-C., Liang, Z., & Zhou, Y.-K. (2023). Interferon-gamma treatment of human umbilical cord mesenchymal stem cells can significantly reduce damage associated with diabetic peripheral neuropathy in mice. Current Stem Cell Research & Therapy.
- Margiana, R., Aman, R. A., Pawitan, J. A., Jusuf, A. A., Ibrahim, N., & Wibowo, H. (2019). The effect of human umbilical cord-derived mesenchymal stem cell conditioned medium on the peripheral nerve regeneration of injured rats. Electronic Journal of General Medicine.
- Ma, Y., Zhou, D., Zhang, H., Tang, L., Qian, F., & Su, J. (2021). Human umbilical cord mesenchymal stem cell-derived extracellular vesicles promote the proliferation of Schwann cells by regulating the PI3K/AKT signaling pathway via transferring miR-21. Stem Cells International.
Use of Umbilical Cord-Derived Mesenchymal Stem Cells (hUC-MSCs) to Treat Spinal Cord Injury (SCI)
Introduction
Spinal cord injury (SCI) is a severe and often life-altering condition that can result in paralysis, loss of sensation, and bowel and bladder dysfunction. Despite the absence of a cure, advances in regenerative medicine have highlighted the potential of mesenchymal stem cells (MSCs), particularly those derived from the umbilical cord (hUC-MSCs), in promoting nerve regeneration and mitigating the effects of SCI (Liu et al., 2024).
What are Mesenchymal Stem Cells?
Mesenchymal stem cells (MSCs) are multipotent adult stem cells capable of differentiating into various cell types, such as bone, cartilage, and muscle cells. MSCs also possess immunomodulatory properties, enabling them to regulate immune responses and reduce inflammation. These characteristics make them promising candidates for treating conditions such as SCI (Rahyussalim et al., 2024).
Why Umbilical Cord-Derived MSCs?
Umbilical cord-derived MSCs have several advantages over other MSC sources. They are easily harvested from discarded umbilical cords, making them ethically uncontroversial. Additionally, hUC-MSCs have a high proliferation rate and express lower levels of human leukocyte antigen (HLA) proteins, reducing the risk of immune rejection. These properties make hUC-MSCs particularly suited for regenerative therapies, including spinal cord repair (Xue et al., 2023).
How Can Umbilical Cord-Derived MSCs Treat SCI?
hUC-MSCs promote tissue repair and regeneration through several mechanisms:
-
Differentiation into nerve cells: hUC-MSCs can differentiate into nerve cells, including oligodendrocytes, which produce myelin, an essential substance for nerve function.
-
Secretion of growth factors: These cells secrete growth factors like brain-derived neurotrophic factor (BDNF) and nerve growth factor (NGF), which support nerve cell survival and regeneration.
-
Immunomodulation: hUC-MSCs can modulate immune responses, reducing inflammation that may contribute to further nerve damage in SCI (Xie et al., 2023).
Clinical Trials Using hUC-MSCs in SCI
Several clinical trials have demonstrated the potential of hUC-MSCs in SCI treatment. For instance, a phase I/II trial in China reported that intravenous administration of hUC-MSCs was safe and well-tolerated, with some patients showing neurological improvements. Another study in Iran confirmed these findings, noting significant improvements in motor function and sensory responses in patients receiving hUC-MSC transplants compared to a placebo group (Liu et al., 2024).
Future Directions
While the use of hUC-MSCs in SCI treatment is still in its early stages, the results from preclinical and clinical studies are promising. However, further research is necessary to determine the optimal dosage, delivery methods, and long-term safety of hUC-MSC therapy for SCI patients. Continued exploration of this treatment could offer hope for individuals affected by spinal cord injuries.
References
-
Liu, J., Wang, H. J., & Chen, X. (2024). Quercetin-loaded human umbilical cord mesenchymal stem cell-derived sEVs for spinal cord injury recovery. Neuroscience. https://typeset.io/papers/quercetin-loaded-human-umbilical-cord-mesenchymal-stem-cell-4b453pv3p7
-
Rahyussalim, A. J., Priyono, A. H., Budhy, F., Muntaha, M., Ramadhani, R., & Canintika, A. F. (2024). Percutaneous laser disc decompression combined with secretome of umbilical cord-derived mesenchymal stem cells in a patient with spinal cord injury: A case report. International Journal of Surgery Case Reports. https://typeset.io/papers/percutaneous-laser-disc-decompression-combined-with-q2ko71vpqc
-
Xue, C., Ma, X., Guan, X., Feng, H., Zheng, M., & Yang, X. (2023). Small extracellular vesicles derived from umbilical cord mesenchymal stem cells repair blood-spinal cord barrier disruption after spinal cord injury through down-regulation of Endothelin-1 in rats. PeerJ. https://typeset.io/papers/small-extracellular-vesicles-derived-from-umbilical-cord-1enrqoi1hx
-
Xie, Y., Sun, Y., Liu, Y., Liu, Q., Xu, J., Qin, Y., He, R., Yuan, F., Wu, T., Duan, C., Jiang, L., Lu, H., & Hu, J. (2023). Targeted delivery of RGD-CD146+CD271+ human umbilical cord mesenchymal stem cell-derived exosomes promotes blood-spinal cord barrier repair after spinal cord injury. ACS Nano. https://typeset.io/papers/targeted-delivery-of-rgd-cd146-cd271-human-umbilical-cord-1o107rlwju
Stem cells have opened the door to a future where we can treat degenerative conditions like Alzheimer’s, Parkinson’s, and spinal cord injuries in ways we never thought possible.
– Shinya Yamanaka (Nobel Prize Winner in Medicine for his work in stem cells)